Early versus Delayed Invasive Intervention in NSTE-ACS: Clinical Outcomes
Abstract
Background: The aim of this study was to compare an early versus a delayed invasive strategy in NSTE-ACS prospectively.
Methods: Prospective observational study including patients admitted for NSTE-ACS requiring an invasive management. The primary endpoint was the occurrence of MACCE (death, new myocardial infarction or stroke) at 30-days and 1-year follow-up.
Results: 167 patients in the early-intervention group (within 24 hours, n = 167) and 129 patients in the delayed-intervention group (24 to 72 hours, n = 129). There was no difference in the primary endpoint of 30-days MACCE (4.2% vs. 6.2%; p = 0.25) and 1-year MACCE (10.2% vs. 17.1%; p = 0.34).
Conclusions: An early invasive strategy does not reduce the risk of death or MACCE compared with a delayed strategy.
Keywords
Non-ST-segment elevation acute coronary syndromes, Timing, Invasive strategy, Clinical outcome
Introduction
In patients with myocardial infarction with ST-segment elevation, in which the infarct-related artery is usually occluded and there is ongoing transmural ischemia, it is well established that the earlier primary percutaneous coronary intervention (PCI) can be performed, the lower the mortality [1,2]. By contrast, in patients with acute coronary syndromes without ST-segment elevation (including unstable angina and myocardial infarction), the culprit artery is often patent, there is usually no ongoing transmural ischemia, and the patient often has a good response to initial medical treatment [3].
Some trials associated early intervention with reduced rates of ischemic events [4,5], others reported higher levels of cardiac injury biomarkers in patients undergoing early invasive treatment [6,7].
The optimal timing of such intervention in many clinical situations has not been well established. Early intervention might prevent ischemic events that could occur while the patient is awaiting a delayed procedure [5]. Alternatively, by treating a patient with intensive antithrombotic therapy and delaying intervention, procedure-related complications might be avoided with intervention on a more stable plaque [6,8].
Our aim was therefore to compare the effects of early invasive intervention with a delayed invasive strategy in our daily practice with a robust clinical primary endpoint of death, re-infarction and stroke at one-year.
Methods
We performed a prospective, observational study to determine the impact of timing of invasive strategy in the clinical outcome of patients with NSTE-ACS.
Patients were enrolled between November 01, 2015 and October 31, 2016 in our cardiology department located in Oran (North-West of Algeria). All patients provided signed informed consent.
Patients aged ≥ 18 years admitted to hospital with NSTE-ACS were eligible to participate. Those with symptoms precipitated by a secondary co-morbidity (e.g., anemia, heart failure, and non-cardiac trauma) and patients participating in concomitant clinical trials were excluded.
Patients were recruited consecutively to avoid selection bias. To be enrolled, patients had to present ischemic symptoms of ACS and have at least one of the following: (1) Electrocardiographic changes (transient ST-segment elevation, ST-segment depression, new T-wave inversion, pseudo-normalization of previously inverted T waves, or (2) An increase in a cardiac biochemical marker of myocardial necrosis (troponin us); (3) Diabetes mellitus.
Patients with persistent ischemia despite medical treatment and with cardiogenic choc, were excluded.
Patients admitted on Sunday, Monday, Tuesday and Wednesday benefited from an early invasive intervention while patients admitted on Thursday, Friday and Saturday benefited from a delayed invasive intervention.
The study was approved by the local ethics committee, and all patients provided written informed consent.
Statistical analyses were performed at the 5% significance level, using 2-sided tests or 2-sided CIs. Continuous data are given as mean and range. Categorical data are summarized using percentages. Logistic regression was performed to test the impact of covariates (e.g., patient characteristics, risk factors, Killip class, risk scores, cardiac biomarkers and angiographic finding) on outcome events. For this analysis, variables were selected as covariates based on a univariate analysis with a significance threshold of 0.20. For the final model, odds ratios and 95% Care given. Data were analyzed with the IBM SPSS Statistics 23.
Results
Patients
From November 2015 through October 2016, we enrolled 296 patients, of whom 167 were randomized to the early-intervention group and 129 to the delayed-intervention group. Complete one-year follow-up was performed in all enrolled patients. Overall, baseline characteristics were similar between the 2 study groups, with more older patients (60.7 years vs. 64 years; p = 0.023), median grace score (123.1 vs. 134.3; p = 0.004) and positive troponin (53.3% vs. 65.9%; p = 0.032) in the delayed intervention group (Table 1). There were no significant differences in the use of in-hospital medication.
The median time from admission to coronary angiography was 17 h 49 min in patients assigned to undergo early intervention and 50 h 51 min in the delayed intervention arm (Table 2). Angiographic baseline characteristics were similar with even distribution of single- and multivessel disease between the 2 groups. Procedural characteristics were similar.
The PCI and CABG rate was similar in the two groups (Table 2).
Primary and secondary outcomes
At 30-day follow-up, the occurrence of the primary endpoint (death, new myocardial infarction or stroke) was 4.2% in early-intervention patients compared with 6.2% in patients undergoing delayed invasive intervention (odds ratio: 1.32, 95% confidence interval: 0.53 to 4.28; p = 0.44) (Table 2). At 30 days, the difference of mortality rates was non-significant (1.8% vs. 3.1%; p = 0.47).
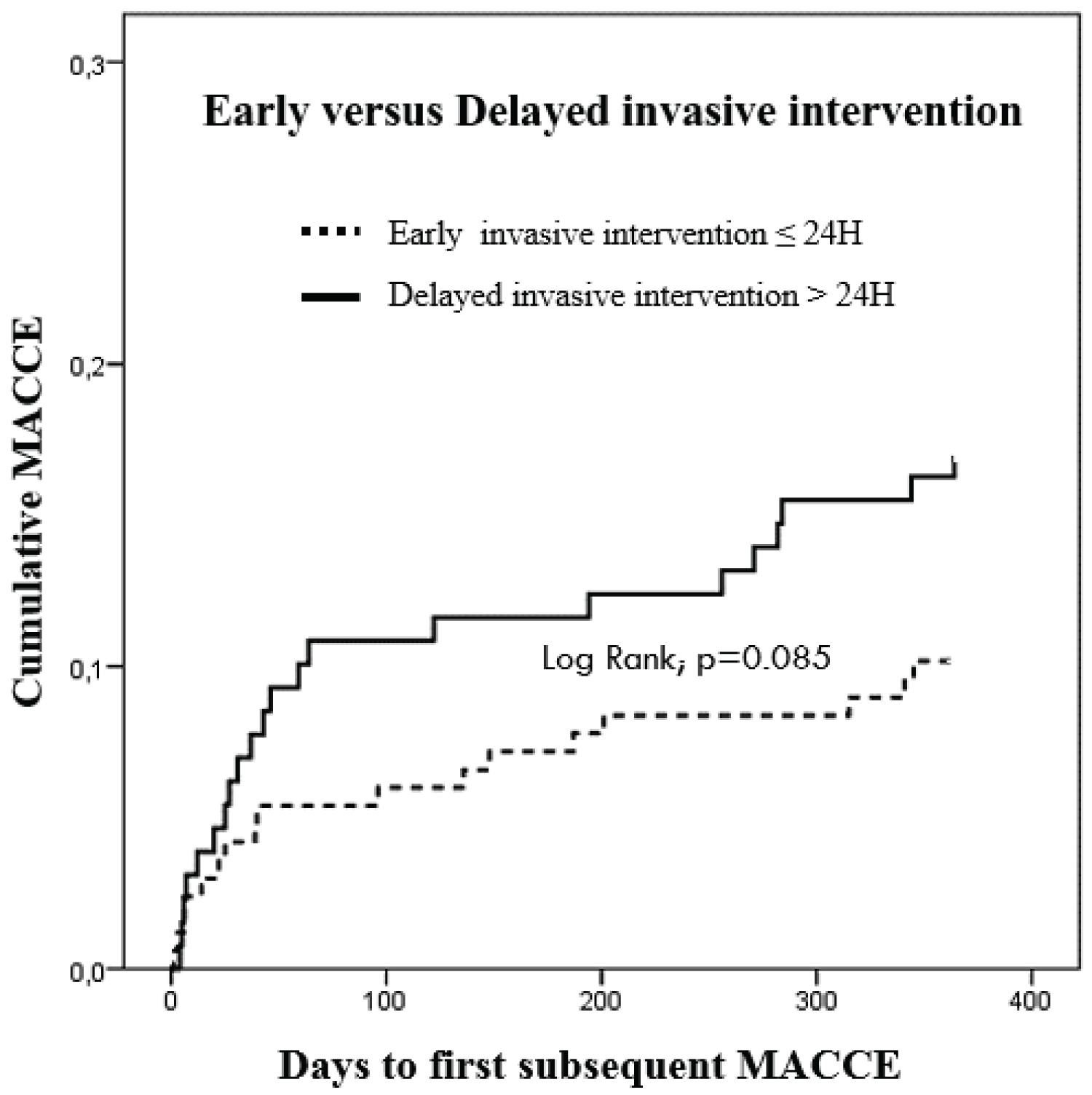
At one-year follow-up, the occurrence of the primary endpoint (death, new myocardial infarction or stroke) was 10.2% in early-intervention patients compared with 17.1% in patients undergoing delayed invasive intervention (odds ratio: 1.8, 95% confidence interval: 0.92 to 3.58; p = 0.087). At one-year, the difference of mortality rates was non-significant (4.2% vs. 7.0%; p = 0.31) (Table 2).
The one-year rates of new MI were 7.8% in patients with early and 11.6% in patients with delayed intervention (p = 0.21) (Table 2).
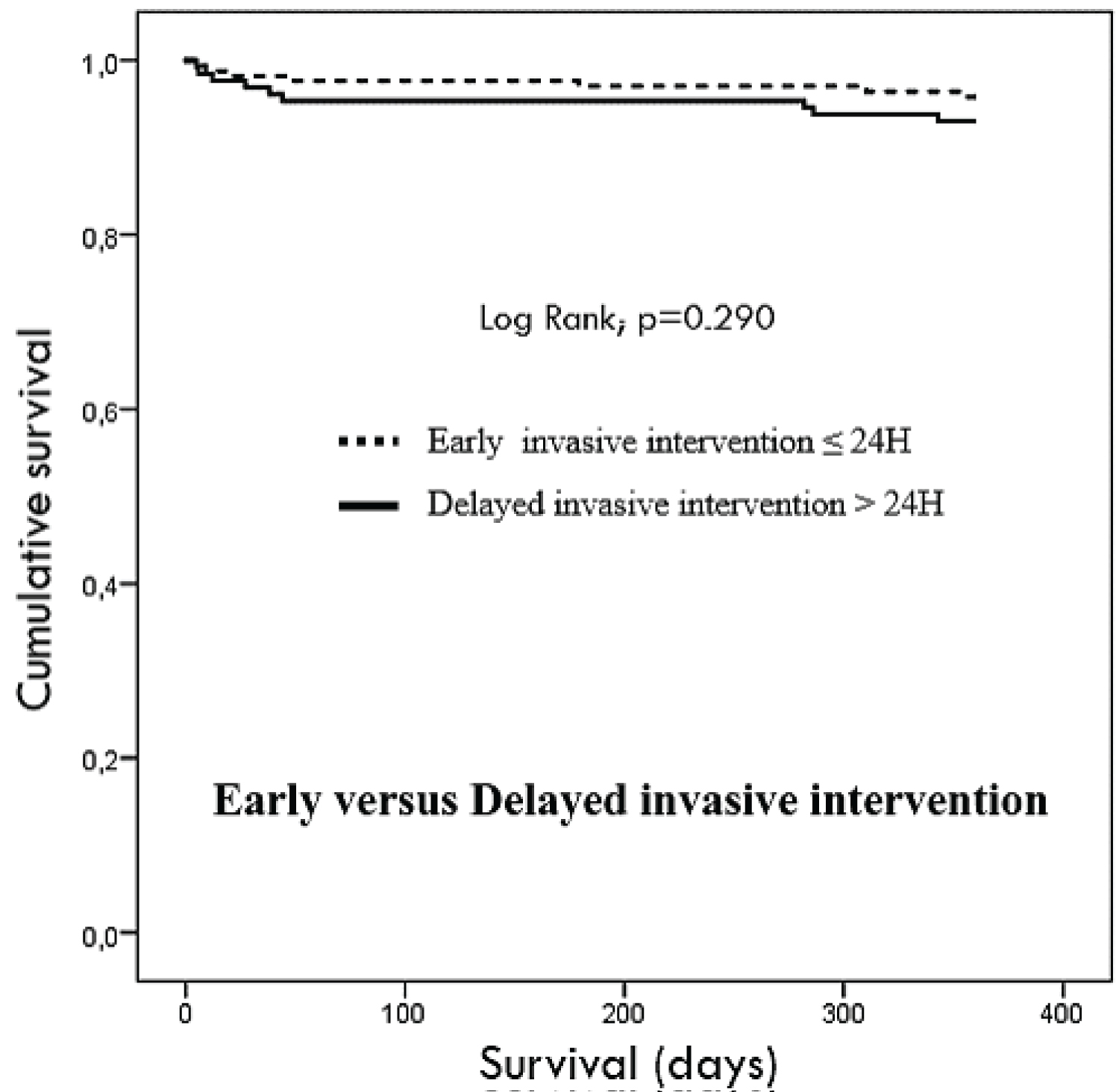
There was no difference in term of survival (Figure 1) and occurrence of MACCE (composite of death, new myocardial infarction and stroke) (Figure 2).
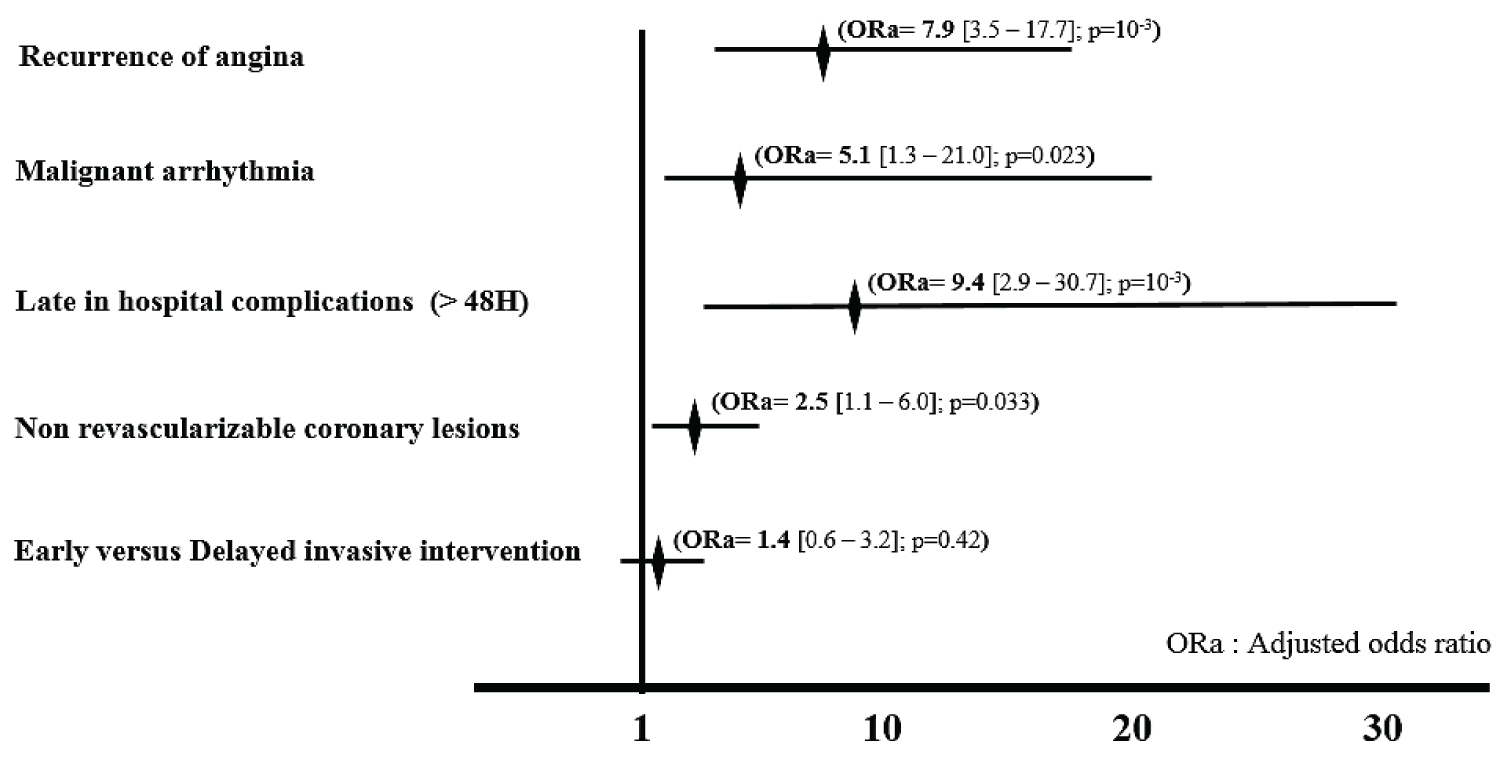
A multivariable regression model constructed to include clinical and procedural information with adjusted odds ratio of 1.4 (95% confidence interval: 0.6 to 3.2; p = 0.42) for the primary endpoint for early versus delayed intervention (Figure 3).
There was no significant interaction between any of the variables (age, grace score and positive troponin) and the assignment to early versus delayed invasive strategy on the primary end point in multivariate regression model.
Bleeding
The occurrence of TIMI major bleeding was low and did not differ between the groups in the in-hospital period (1.8% vs. 3.1%; p = 0.47) (Table 2).
In-hospital stay: The patients of early invasive intervention had shorter in-hospital stay (103 h vs. 142 h; p < 10-3) (Table 2).
Discussion
The principal findings of our study are that in patients with acute coronary syndromes without ST-segment elevation, an early-intervention strategy was not superior to a delayed-intervention strategy for the prevention of death, myocardial infarction, or stroke. However, an early-intervention strategy significantly reduced the in-hospital stay.
Although meta-analyses of previous randomized trials that compared an invasive strategy with a conservative strategy in patients with acute coronary syndromes have shown a benefit for an invasive strategy, [9] the timing of angiography in the invasive-strategy group of these previous studies ranged from as early as 19 hours after randomization in one large trial [8] to as late as 96 hours in another large trial [10]. Given this wide variation in the timing, there remains substantial uncertainty regarding the optimal timing for intervention in such patients. Although some observational analyses have suggested that earlier intervention, as compared with delayed intervention, may reduce events, [11] others have suggested that outcomes appear to be similar between the two approaches [12].
Study population
Our trial included NSTE-ACS patients with a proportion of 58.8% of NSTEMI. In addition, 71.3% of patients in our study had ST-segment depression on admission, which is higher compared with previous trials [5,6,13], and 50% underwent percutaneous or surgical revascularization, which is similar or less to previous studies [5,11].
The lack of a significant difference in the rate of death, myocardial infarction, or stroke in the overall population between these two invasive strategies suggests that most patients with acute coronary syndromes can be treated safely with either early intervention or delayed intervention. The results of our study provide reassurance that patients who are not at high risk can undergo interventions less urgently.
A potentially important finding in our study was that despite delayed patients group were older with more important mean Grace score and more positive troponin, the primary and secondary end-points was non-different between the two groups.
A limitation of our study was that even with a sample size of less than 300 patients, the trial may have been relatively underpowered. A strength of the trial was that since the primary outcome focused on hard clinical outcomes, our results offer important information for the practicing clinician regarding the appropriate timing of intervention in patients with acute coronary syndromes.
Conclusion
In summary, our study showed that in most patients with acute coronary syndromes without ST-segment elevation, an early-intervention strategy did not differ from a delayed-intervention strategy in preventing a composite outcome of death, myocardial infarction, or stroke. However, early intervention significantly reduced the in-hospital stay.
Acknowledgements
I am grateful to all of those with whom I have had the pleasure to work during this project.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
References
- Cannon CP, Gibson CM, Lambrew CT, et al. (2000) Relationship of symptom-onset-to balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283: 2941-2947.
- Antman EM, Hand M, Armstrong PW, et al. (2008) 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task force on practice guidelines. Circulation 117: 296-329.
- Fuster V, Badimon L, Badimon JJ, et al. (1992) The pathogenesis of coronary artery disease and the acute coronary syndromes. N Engl J Med 326: 310-318.
- Zhang J, Qiao SB, Zhu J (2010) Outcome of patients with non-ST segment elevation acute coronary syndrome undergoing early or delayed intervention. Zhonghua Xin Xue Guan Bing Za Zhi 38: 865-869.
- Neumann FJ, Kastrati A, Pogatsa-Murray G, et al. (2003) Evaluation of prolonged antithrombotic pretreatment ("cooling-off" strategy) before intervention in patients with unstable coronary syndromes: A randomized controlled trial. JAMA 290: 1593-1599.
- Riezebos RK, Ronner E, Ter Bals E, et al. (2009) Immediate versus deferred coronary angioplasty in non-ST-segment elevation acute coronary syndromes. Heart 95: 807-812.
- van’t Hof AW, de Vries ST, Dambrink JH, et al. (2003) A comparison of two invasive strategies in patients with non-ST elevation acute coronary syndromes: Results of the Early or Late Intervention in unstable Angina (ELISA) pilot study. 2b/3a upstream therapy and acute coronary syndromes. Eur Heart J 24: 1401-1405.
- de Winter RJ, Windhausen F, Cornel JH, et al. (2005) Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med 353: 1095-1104.
- Li Y, Zhang Z, Xiong X, et al. (2017) Immediate/Early vs. delayed invasive strategy for patients with Non-ST-segment elevation acute coronary syndromes: A systematic review and meta-analysis. Front Physiol 8: 952.
- (1999) Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomized multicentre study. Lancet 354: 708-715.
- Mehta SR, Granger CB, Boden WE, et al. (2009) Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med 360: 2165-2175.
- The Fifth organization to assess strategies in acute ischemic syndromes investigators, Salim Yusuf, Shamir R Mehta, et al. (2006) Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med 354: 1464-1476.
- Thiele H, Rach J, Klein N, et al. (2012) Optimal timing of invasive angiography in stable non-ST-elevation myocardial infarction: The Leipzig Immediate versus early and late Percutaneous coronary Intervention triAl in NSTEMI (LIPSIA-NSTEMI trial). Eur Heart J 33: 2035-2043.
Corresponding Author
Farouk Boukerche, Interventional Cardiology Unit, Department of Cardiology, Oran Faculty of Medicine, Oran University, Ahmed Benbella, Algeria, Tel: 00213770352195
Copyright
© 2022 Boukerche F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.