A Focused Review on the Approach to the Recurrent Laryngeal Nerve & Identification during Thyroidectomy
Abstract
Thyroid surgeries are the most frequently performed endocrine procedures worldwide. The recurrent laryngeal nerve (RLN) shows some anatomical variations that can potentially compromise the safety of thyroid surgery, Hence, Thyroid surgeons should have a number of different techniques available in the event that identification of the RLN proves troublesome. Moreover, sufficient knowledge of surgical anatomy, clinical experience, and meticulous surgical techniques are key factors in the identification and safe dissection of the RLN. In this article, we will discuss the Anatomy & variations in Recurrent Laryngeal Nerve, possible approaches to identify it & how to minimize the incidence of inadvertent injury to the nerve.
Keywords
Recurrent laryngeal nerve, Thyroid surgery, Zuckerkandl tubercle
Introduction
Thyroid surgeries are the most frequently performed endocrine procedures worldwide. One of the most serious complications of thyroid surgery is injury to the recurrent laryngeal nerve (RLN), which varies from 0.5% to 14.0%, depending on the type of disease, the type of surgery, the extent of resection, and the surgical technique [1-3].
Classically a bilateral subtotal thyroidectomy was performed to minimize operative risk and Leave a small portion of functioning tissue [4]. Unfortunately, subtotal thyroidectomy carries a considerable lifelong risk of recurrence for some patients after a long interval. After subtotal resection of multinodular goiter, rates of up to 40% have been reported for recurrent goiter at long-term followup [5].
RLN injury during thyroidectomy can result from transection, clamping, stretching, electrothermal injury, ligature entrapment, or ischemia [6]. Moreover, Anatomical integrity of the RLN does not indicate intact function [7].
The risk factors that increase RLN injury during thyroidectomy are primary or recurrent malignant diseases, recurrent benign diseases, thyrotoxicosis, the extent of the surgery, routine non-observance of RLN (no RLN dissection), low-volume hospital or surgeon, substernal goiter, nerve branching, aberrant course of the nerve, and presence of non-RLN [8-10].
The use of intraoperative nerve monitoring is a luxury that cannot be afforded by many centers and hence there is a need for easy nerve identification in a way that the surgeon finds most convenient.
Thyroid surgeons should have a number of different techniques available in the event that identification of the RLN proves troublesome. Sufficient knowledge of surgical anatomy, clinical experience, and meticulous surgical techniques are key factors in the identification and safe dissection of the RLN.
A Brief History of Thyroid Surgery Evolution
In 1846, Robert Liston called thyroid surgery 'a proceeding by no means to be thought of' after performing five thyroidectomies [11]. Halsted in his 'The operative history of goiter' scrutinized procedures done before 1850 and analyzed them to be associated with 40% mortality. The high mortality was due to hemorrhage, asphyxia due to tracheal compression, hospital gangrene and air embolism [12].
The parathyroid blood supply was published in 1907 by Halsted and Evans. They opined that 'ultra-ligation' of the thyroid arteries was to be practiced, which was ligation distal to the points of origin of the parathyroid artery branches. They suggested avoiding inferior thyroid artery ligation [13].
In 1909, Kocher was awarded the Nobel Prize for his thyroid surgery new era. At the age of 76, in 1917, he presented the results of his work at the Swiss Surgical Congress. His presentation revealed about 500 thyroid surgeries performed by him with a mortality rate of 0.5% [14]. First described by Kocher in 1912, thyroidectomy has become a routinely performed surgery [15], Moreover, Galen described the RLN. Surgeons including Billroth, Kocher, and Joll tried to avoid dissection near it; though others like Lahey favored to expose the RLN [16].
Relevant Anatomy, Variations of RLN and Proposed Triangles
The Thyroid Anatomy has been illustrated extensively in the literature that's beyond the scope of this article. We will review the RLN surgical anatomy & its landmarks in the neck. Visual identification of the RLN remains the gold standard for RLN injury prevention [17], a thyroid surgeon should be aware of the surgical anatomy, different variations & its lighthouses.
The right RLN arises from the vagus at a level where the brachiocephalic artery is divided into Righ Subclavian & Right common carotid Arteries, rotates backward around the right subclavian artery and advances toward the tracheoesophageal groove after passing behind the carotid artery at an angle of about 35° with the trachea before entering into the larynx deep to the inferior constrictor muscle [18].
The left RLN arises from the vagus at the level of the ligamentum arteriosum and turns backward around aortic arch and reaches the tracheoesophageal groove from the medial to the left common carotid artery. Because the angle between the left RLN and the trachea about 15°, it is localized deeper than the right RLN and communicates with the tracheoesophageal groove more inferiorly. Furthermore, the left RLN is approximately 2 times longer than the right RLN due to different levels of origin from the vagus nerve. In general, the left RLN route is longer than the right, while the right nerve is more oblique than the left as it ascends [3,18,19].
Non-recurrent laryngeal nerve
The nerve arising from the upper part of the vagus reaches the larynx without turning around the main vessels. This anomaly is defined as non-recurrent laryngeal nerve (non-RLN) and was found on the right side in 0.7% of the cases in the clinical series and 1.4% in cadaver studies. On the left side, non-RLN is very rare and is associated with situs inversus [20].
Zuckerkandl tubercle
The Zuckerkandl Tubercle (ZT) is a lateral or posterior projection, considered to be the fusion point of the ultimabranchial body (lateral thyroid body) and the median thyroid, and may become prominent. It is located between the superior and inferior poles, pointing toward the tracheoesophageal groove [21].
It is classified as grade 1 if it is observed as a consolidation of the lateral margin of the thyroid lobe, as grade 2 if it is smaller than 1 cm, and grade 3 if it is greater than 1 cm. 63%-77% of thyroidectomies were reported to have an enlarged ZT, and it was found that the RLN mostly (93%) courses medially and rarely, (7%) laterally to the ZT [22].
Gurleyik, et al. stated that a large ZT is present in 51% of thyroid lobes, and RLN was laying on the anterior, lateral surface of the ZT in 6% of instances. The incidence of a superficial, lateral course of the RLN has been reported as 6%-7% in primary thyroidectomy cases [23].
Gravante, et al. stated The nerve lies in front when the ZT is very small or when there is only thickening of the lateral edge of the thyroid lobes; more frequently the nerve runs in a tunnel deep behind the tubercle [24].
Berry's ligament
Berry's ligament is consolidation of the pretracheal fascia connects the thyroid to the cricoid cartilage and the first 2 tracheal rings. The distance between the site of attachment to the cricoid cartilage and the entry of the RLN is 1.9 mm in average. At the last 2 cm of the RLN, the Berry's ligament lies medial to the RLN [19].
A superficial vascular fascia covers the upper aspect of the RLN, which is observed when the lobe is rotated anteromedially during thyroidectomy. It contains the delicate tertiary artery, branches of veins of the thyroid gland, including the ZT and the upper parathyroid gland. When this structure is opened, the RLN becomes visible in the tracheoesophageal groove [25].
Thyroid tissue may occasionally extend posteriorly toward the RLN. If this is the case for a benign thyroid lesion, no further dissection should be performed, and it should be left at the site under the RLN [26].
To complete the anatomical picture, The External Branch of Superior Laryngeal Nerve (EBSLN) passes along the dorsal aspect of the carotid sheath after it is branched out of SLN. While it runs parallel to the superior thyroid artery, it descends into the cricothyroid muscle to supply. During this descent, it may course beneath the superficial pretracheal fascia covering the lateral aspect of the inferior pharyngeal constrictor muscle either above the muscle, or under or between the muscle fibers [27].
The EBSLN runs 1-2 mm immediately posterior to the oblique insertion site of the laryngeal tip of the sternothyroid muscle to the thyroid cartilage in intimate relation to the upper thyroid pole [27].
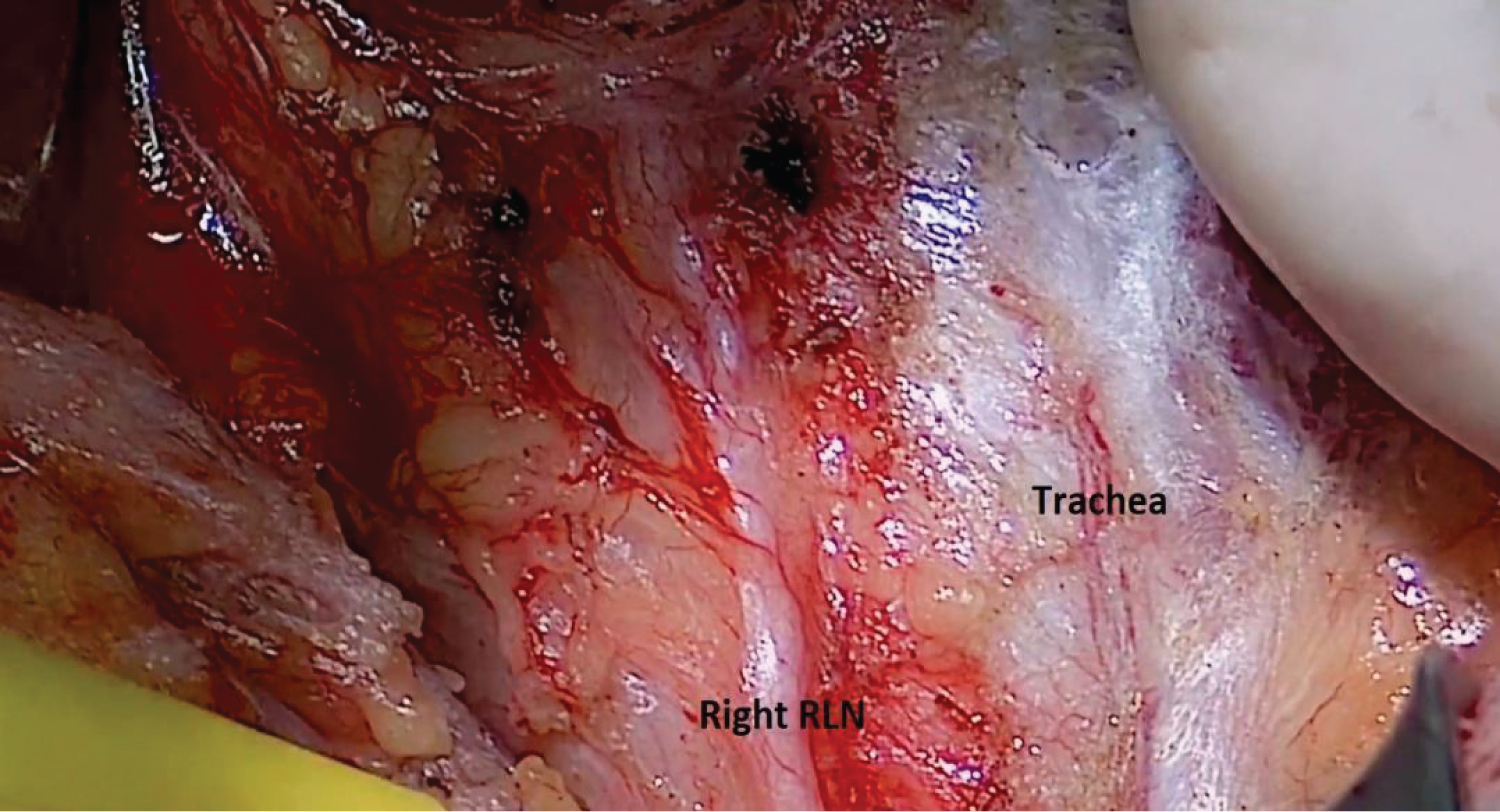
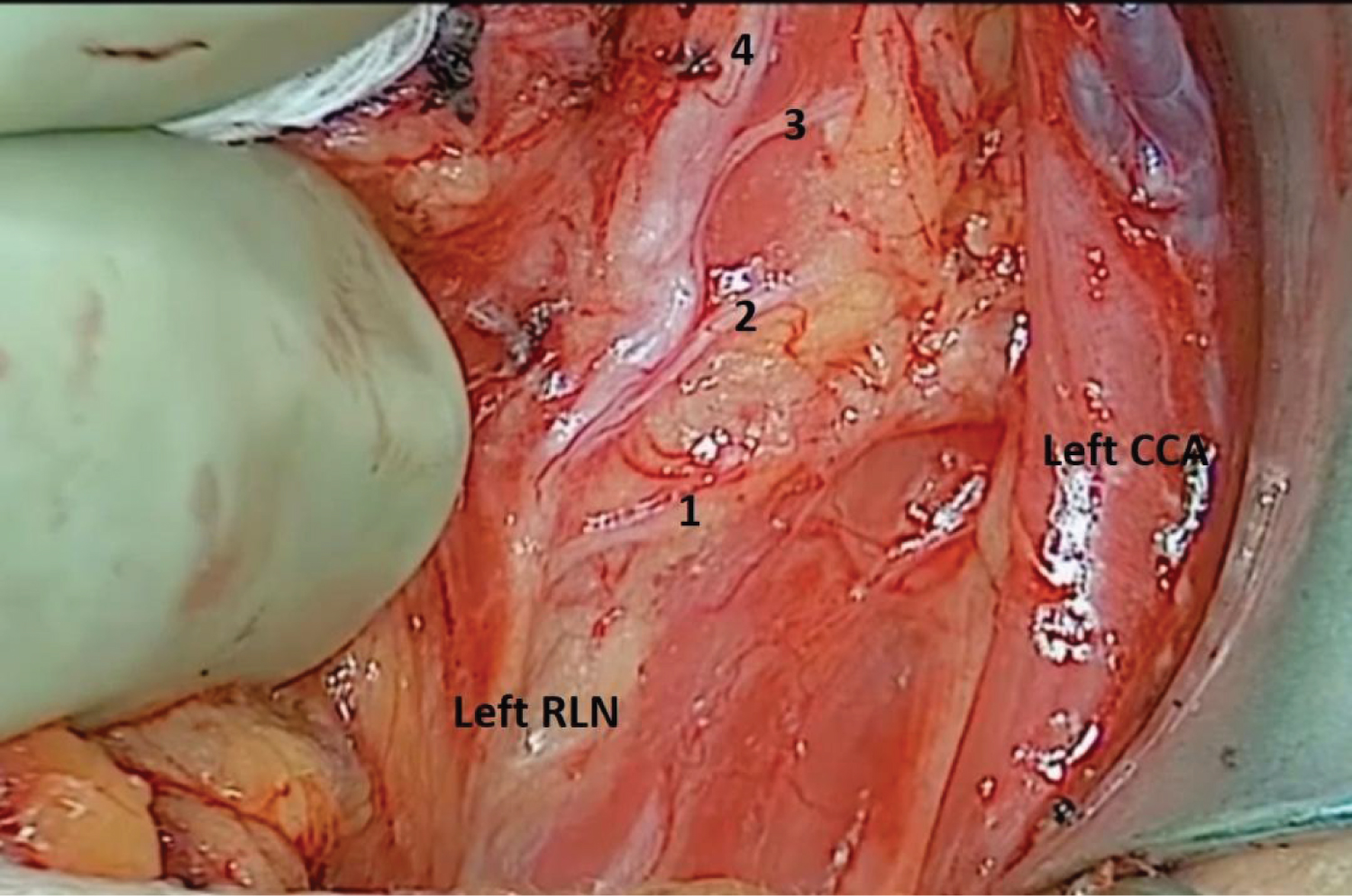
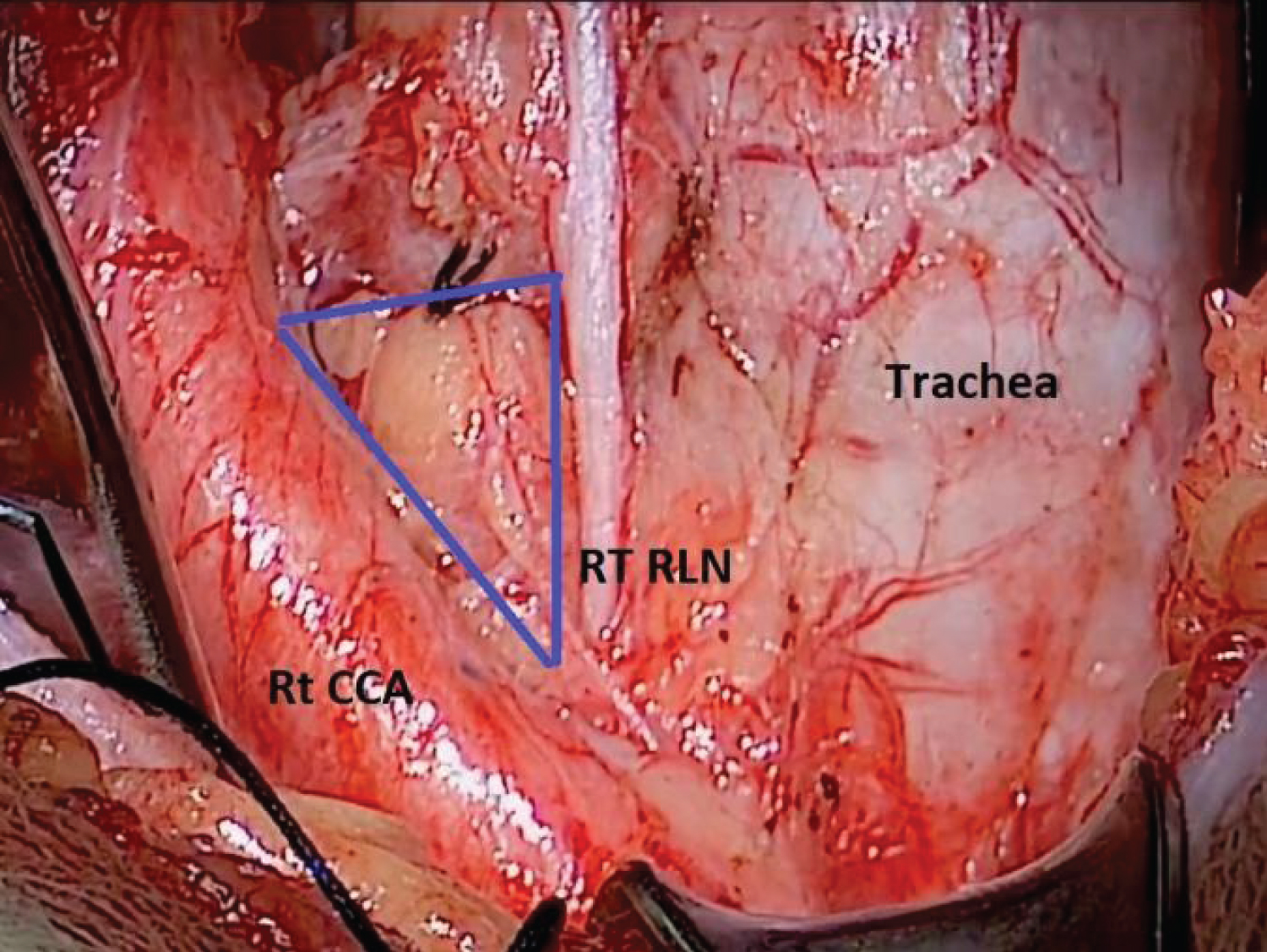
The recurrent laryngeal nerve (RLN) shows some anatomical variations that can potentially compromise the safety of thyroid surgery. The extralaryngeal branching of the RLN is a common anatomical variation encountered in thyroid surgery and represents a source of increased surgical morbidity (Figure 1, Figure 2 and Figure 3). In some reports, extralaryngeal branching of the RLN occurs with up to 36% with the branching of the RLN into two or more divisions on one or both sides [28].
Seven RLN anatomical variations were identified in a Chinese study enrolled 2,404 patients undergone hemi or total thyroidectomies, 690 (21.1%) RLNs exhibited anatomical variations. Shao T, et al. observed a significantly higher rate of anatomical variation of the right RLN compared with the left RLN (Table 1). The right RLN tends to be more variable in its position, both in relation to the inferior thyroid artery and also in being more anterolateral than the left RLN, which almost always tends to lie in the trachea-oesophageal groove. This could be explained by the embryological origin of the RLN [29].
Transient post-operative RLN paralysis occurs in approximately 3-8% of cases and permanent paralysis in 0.3-3% of cases [30-32]. Visual identification of the RLN remains the gold standard for RLN injury prevention [17].
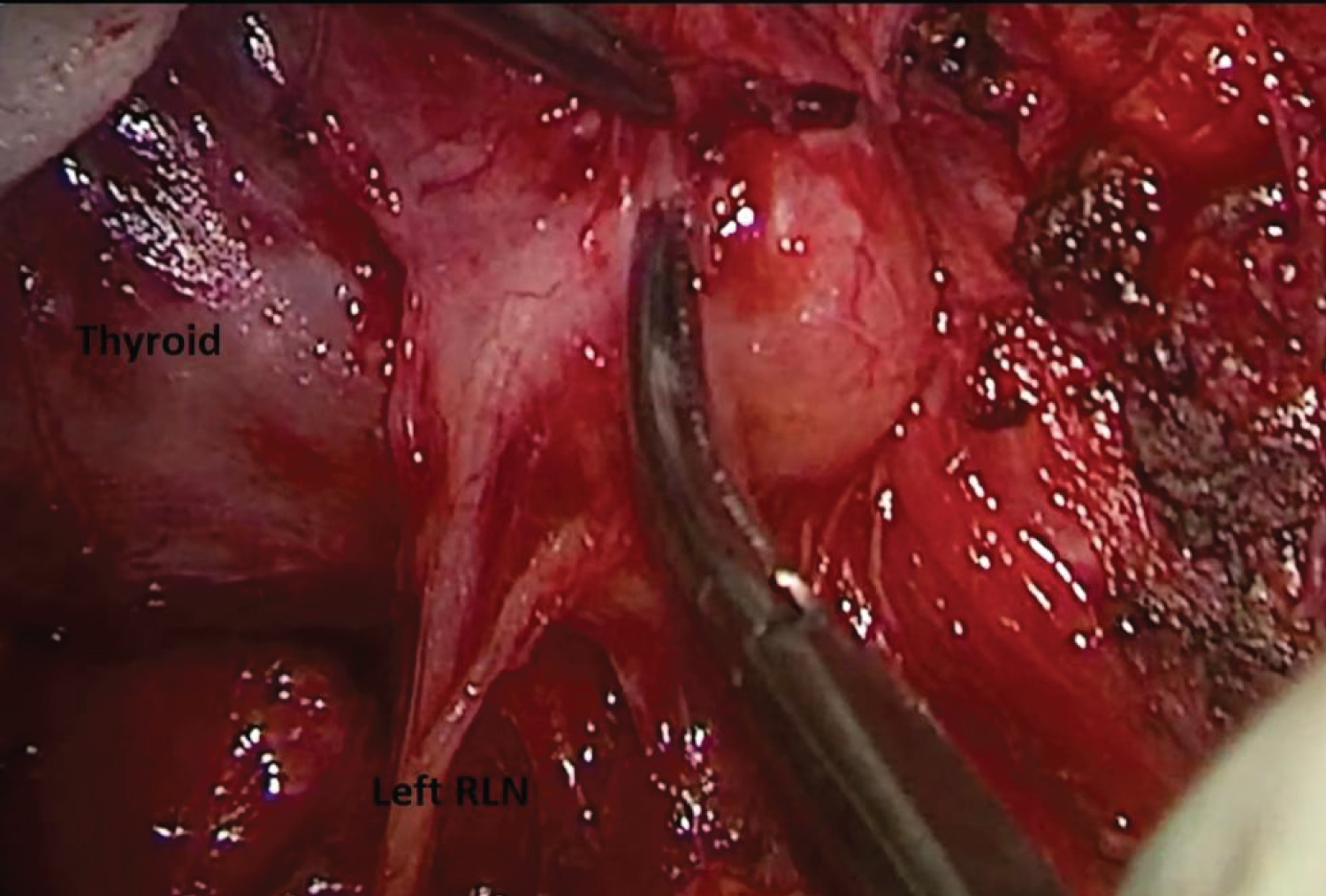
Emin Gurleyik, et al. studied the Recurrent Laryngeal Nerve displacement post redo thyroidectomy, 26.2% of exposed RLNs were identified at both lateral and superficial locations in the thyroid bed according to remnant tissue. They commented that in reoperations the RLN could be displaced laterally and located adherent to the lateral capsule of the remnant thyroid. In this position, the nerve is stretched by the enlarged remnant and may be mistaken for fibrotic bands, thin ligaments, and blood vessels, thereby increasing the risk of inadvertent transection if not identified properly [33] (Figure 4).
The Intra-Operative Nerve Monitoring (IONM) provides intraoperative information about RLN function and helps to predict its postoperative functional status. Wojtczak, et al., have reported that final confirmation of RLN functionality is crucial in cases where the RLN runs over a recurrent goiter because the nerve is particularly prone to overstretching with the potential loss of function after dissection [34].
Many Anatomical triangles were described to assist in identification of the RLN in the surgical practice.
Beahr's Triangle or Riddle's triangle: This triangle is named after OH Beahrs. Also synonym with Riddle's triangle, the nerve is identified proximal in the tracheo-oesophageal groove. The nerve forms the third side of Beahr's triangle. The other two sides are by the common carotid and inferior thyroid arteries [35] (Figure 5).
Simon's triangle: Anterior border is formed by the recurrent laryngeal nerve, posterior by the common carotid artery and base is formed by the inferior thyroid artery [36].
Lore's triangle
Medial border is by the trachea/esophagus, laterally the carotid artery and superiorly the surface of inferior pole of thyroid [37].
Triangle of concern: The sites of bleeding during thyroidectomy are middle thyroid veins, inferior thyroid veins and branches of inferior thyroid artery in the vicinity of RLN [36].
Cricothyroid space of reeves: This is an avascular space between the upper pole of the thyroid and the cricothyroid muscle which is useful in dissection and helps in avoiding injury to the superior laryngeal nerve [36].
Joll's triangle: Synonym is sternothyrolaryngeal triangle. This is used to identify external branch of superior laryngeal nerve which lies within this triangle. Upper pole of thyroid gland and superior thyroid vessels forms the Lateral border. Superiorly, Attachment of the strap muscles, Medially is the Midline, The floor is formed by Cricothyroid muscle [38].
Hermann, et al. found that the number of injuries significantly decreased with visual identification of the RLN. They found that complete dissection is highly superior to partial exposure of the nerve [39]. After the RLN is observed, a minimal dissection from the medial aspect of the RLN should be performed, if possible. Care must be taken to protect the nerve's vaso-nervosums, and energy devices should not be used near the nerve. Forceful aspiration and compression with gauze tampons should not be applied. The use of magnifying glasses with sufficient light also significantly contributes to dissection [40].
The resection of an enlarged remnant gland and reoperations in the thyroid bed are surgically challenging because of the distortion of anatomic planes and scarring from previous surgeries [4]. Thyroid re-operations can be challenging, even for a highly experienced thyroid surgeon, as visual identification of the RLN is more difficult during dissection of scar tissue than in the virgin neck [9].
Approaches to Recurrent Laryngeal Nerve during Thyroidectomy
There are 4 different described approaches in the literature to access the RLN, will summarize them here.
Lateral approach
This technique is often applied to primary thyroid surgery, the thyroid and strap muscles are first dissected away and the lateral thyroid veins are ligated, then releasing the upper pole initially will provide an additional field. Usually, the strap muscles and carotid artery are retracted laterally and the thyroid anteromedially to expose the paratracheal region where the RLN is anatomically located. Usually the superior parathyroids lie posterior to the RLN while the inferior parathyroids lie anterior to it, also the inferior horn of the thyroid cartilage can be used as a guide. The RLN is usually found by dissection around the inferior thyroid artery at the level of the middle pole of the thyroid [41,42].
This approach can be challenging in cases of large goiters or a large ZT. In secondary surgeries, searching for the nerve within this area may be risky, due to dense scar tissue. Also, in the presence of non-RLN, the lateral approach may is not advised as the nerve courses perpendicularly to its normal course in secondary cases [43].
Medial approach
It's preferred for substernal or enlarged retropharyngeal goiters. The isthmus is first divided to reveal the anterolateral part of the trachea. Identification of the cricothyroid muscle and dissect between it & the medial part of the superior thyroid pole. The fibers between the trachea and the thyroid, and the Berry ligament fibers are gradually divided starting from the second tracheal ring, then visualizing the RLN from the medial aspect of the thyroid and the lateral aspect of the trachea [26].
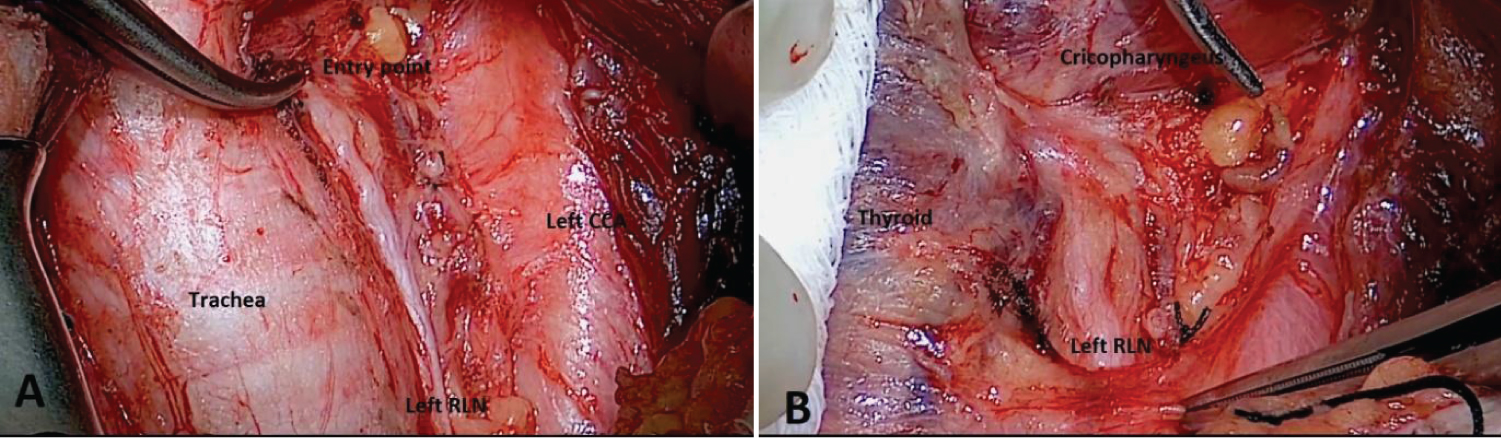
If the RLN is displaced posteriorly, it may not be detected with this approach. In this case, the upper pole is dissected and pulled in a lateral direction; exposing the cricopharyngeal muscle at the fixed entry point of RLN [26].
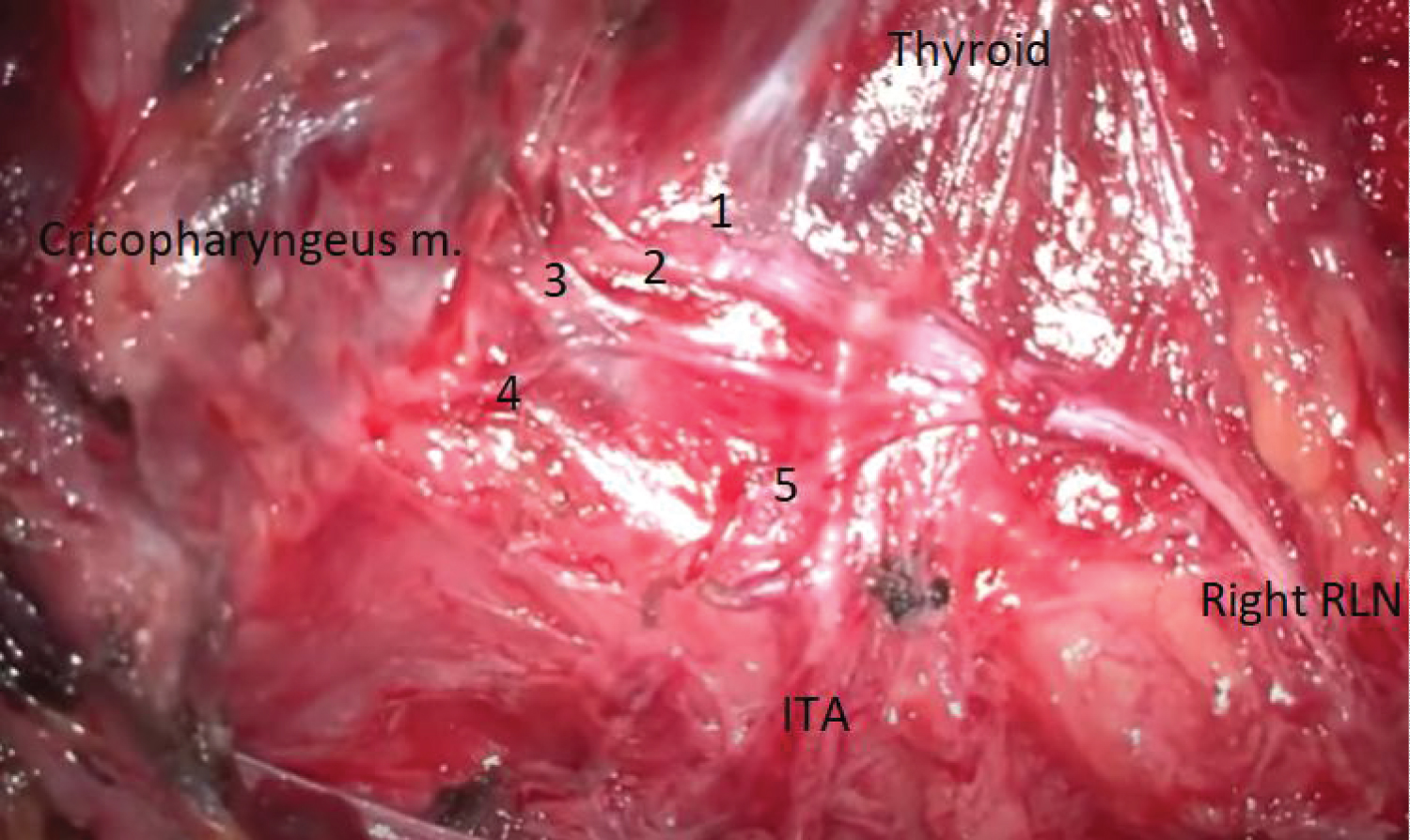
Superior approach
It's also called the medial superior approach and may be recommended for patients with huge goiters or large substernal goiters because releasing the lobe through inferior or lateral approach is quite challenging. It's also suitable for non-RLN suspected cases or when RLN is not found with the other approaches. The most important anatomical hallmark in this approach is the lower border of the cricopharyngeal muscle, deep to it, RLN enters to the larynx. In all these cases, the position of the RLN at this point is fixed & consistent [43] (Figure 6).
The upper pole of the thyroid is released, pulled forwards and laterally to expose the cricothyroid and cricopharyngeal muscles to reveal the laryngeal entry point of the RLN [43].
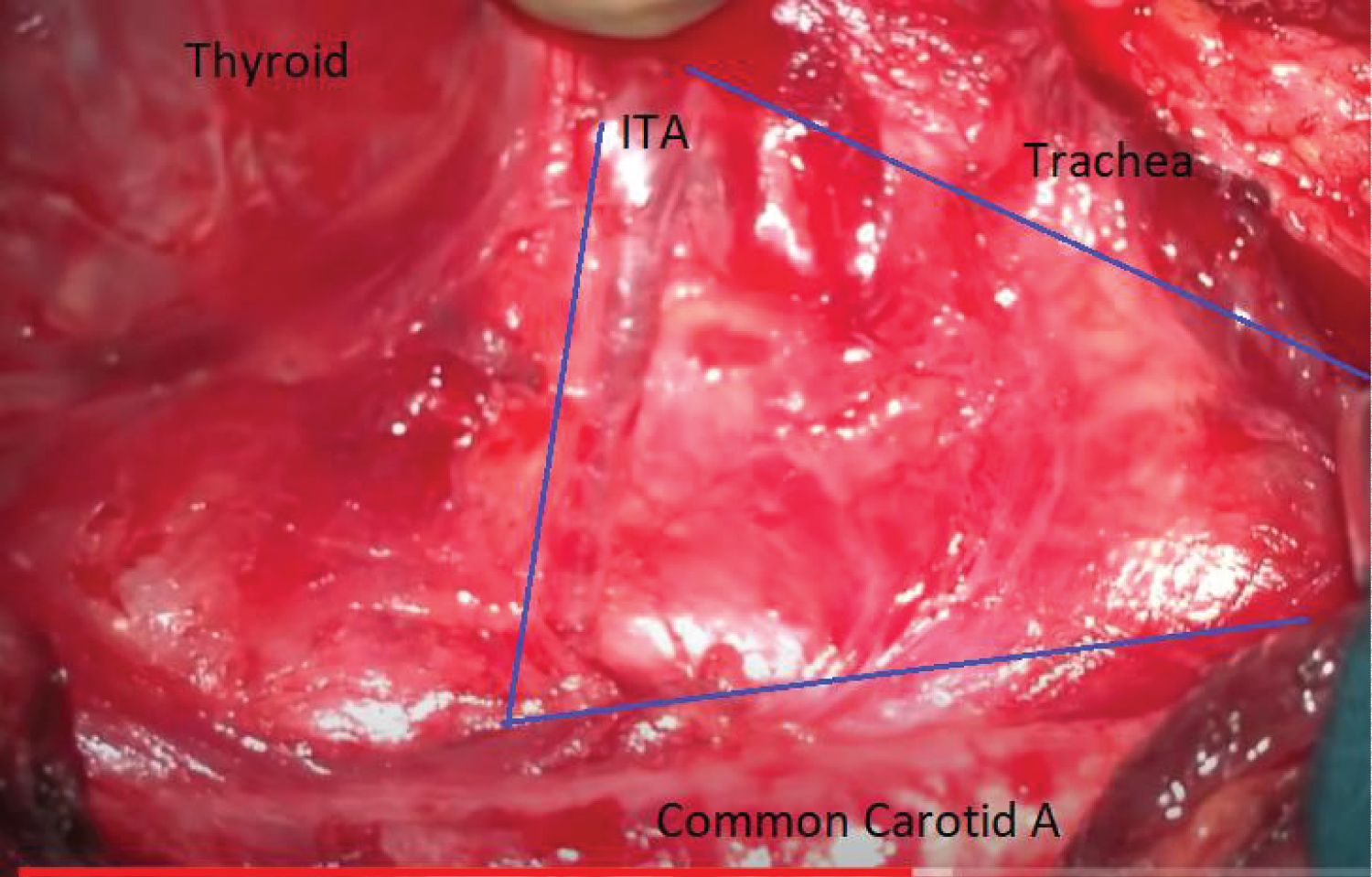
Inferior approach
This approach entails detection of the RLN from its entry in the 'virgin' thoracic outlet region devoid of scar tissue during secondary surgical procedures [19].
This area is known as the RLN triangle, According to the definition of Lore, et al., the thoracic entry forms the top of the triangle, the common carotid artery (or strap muscles) forms the lateral margin, the trachea and esophagus form the medial margin, and the lower border of the inferior lobe of the thyroid forms the base [37] (Figure 7).
Because the entrance of the RLN to the thyroid area differs, the RLN is sought at an area more lateral to its thoracic inlet on the right side, whereas it is sought closer to the paratracheal area on the left side [43]. Extralaryngeal branching is rare in this region, and the RLN is present as a single trunk, and thus, its laryngeal course may be easily visualized. However, it is stated that the dissection in the long segment may increase the risk of nerve injury [37].
In addition, because the inferior parathyroid vessel runs in a lateral to medial direction, the risk of parathyroid devascularization may increase. In order to avoid this, after identifying the RLN, the fatty tissue area through which the parathyroid vessel passes is bypassed and the dissection is continued toward the cranial region [29]. The inferior approach is not appropriate for patients with large substernal goiters and in the presence of non-RLN.
In case of a Re-do thyroidectomy, where anterior approach is not feasible, tightly adhered, the RLN can be accessed by a "back door" approach after medial reflection of the sternohyoid & sternothyroid muscles & lateral traction of Sternomastoid muscle [43].
Disclosure of Interest
The authors declare they have no conflicts of interest related to this article.
Conclusion
In conclusion, a "perfect" technique for thyroidectomy cannot be described, since every thyroid surgeon is bearing a morbidity rate that cannot reach the 0%. Nevertheless, this rate can be "kept to a minimum" when a thorough knowledge of surgical anatomy & a safe surgical technique are followed. The surgeon should keep in mind that different surgical approaches need to be entertained according to different scenarios.
References
- Randolph GW, Kobler JB, Wilkins J (2004) Recurrent laryngeal nerve identification and assessment during thyroid surgery: Laryngeal palpation. World J Surg 28: 755-760.
- Hepgul G, Kucukyilmaz M, Koc O, et al. (2013) The identification of recurrent laryngeal nerve by injection of blue dye into the inferior thyroid artery in elusive locations. J Thyroid Res 2013: 539274.
- Kaisha W, Wobenjo A, Saidi H (2011) Topography of the recurrent laryngeal nerve in relation to the thyroid artery, Zuckerkandl tubercle, and Berry ligament in Kenyans. Clin Anat 24: 853-857.
- Richer SL, Wenig BL (2008) Changes in surgical anatomy following thyroidectomy. Otolaryngologic Clinics of North America 41: 1069-1078.
- Thomusch O, SekullaC, Dralle H (2003) Is primary total thyroidectomy justified in benign multinodular goiter? Results of a prospective quality assurance study of 45 hospitals offering different levels of care. Der Chirurg 74: 437-443.
- Dralle H, Sekulla C, Haerting J, et al. (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136: 1310-1322.
- Chiang FY, Lu IC, Chen HC, et al. (2010) Anatomical variations of recurrent laryngeal nerve during thyroid surgery: How to identify and handle the variations with intraoperative neuromonitoring. Kaohsiung J Med Sci 26: 575-583.
- Bergenfelz A, Salem AF, Jacobsson H, et al. (2016) Risk of recurrent laryngeal nerve palsy in patients undergoing thyroidectomy with and without intraoperative nerve monitoring. Br J Surg 103: 1828-1838.
- Barczy´nski A, Konturek K, Pragacz A, et al. (2014) Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: Results of a retrospective cohort study. World J Surg 38: 599-606.
- Sancho JJ, Pascual-Damieta M, Pereira JA, et al. (2008) Risk factors for transient vocal cord palsy after thyroidectomy. Br J Surg 95: 961-967.
- Liston R (1846) Lectures on the operations of surgery and on diseases and accidents by Thomas D. Mutter. Lee & Blanchard, Philadelphia.
- Desault PJ (1792) Giraud. Jour De Chir De Paris 3: 3.
- Halsted WS, Evans HM (1907) I. The parathyroid glandules. Their blood supply and their preservation in operations upon the thyroid gland. Ann Surg 46: 489-506.
- Becker WF (1977) Presidential address: Pioneers in thyroid surgery. Ann Surg 185: 493-504.
- McGreevy PS, Miller FA (1969) Biography of Theodor Kocher. Surgery 65: 990-999.
- Lahey FH (1944) Exposure of recurrent laryngeal nerves in thyroid operations. Surg Gynecol Obstet 78: 293.
- Page C, Monet P, Peltier J, et al. (2008) Non-recurrent laryngeal nerve related to thyroid surgery: Report of three cases. The Journal of Laryngology and Otology 122: 757-761.
- Tang WJ, Sun SQ, Wang XL, et al. (2012) An applied anatomical study on the recurrent laryngeal nerve and inferior thyroid artery. Surg Radiol Anat 34: 325-332.
- Fundakowski CE, Hales NW, Agrawal N, et al. (2018) Surgical management of the recurrent laryngeal nerve in thyroidectomy: American Head and Neck Society Consensus Statement. Head Neck 40: 663-675.
- Henry BM, Sanna S, Graves MJ, et al. (2017) The non-recurrent laryngeal nerve: A meta-analysis and clinical considerations. Peer J 5: e3012.
- Pelizzo MR, Toniato A, Gemo G (1998) Zuckerkandl's tuberculum: An arrow pointing to the recurrent laryngeal nerve (constant anatomical landmark). J Am Coll Surg187: 333-336.
- Gauger PG, Delbridge LW, Thompson NW, et al. (2001) Incidence and importance of the tubercle of Zuckerkandl in thyroid surgery. Eur J Surg 167: 249-254.
- Gurleyik E, Gurleyik G (2012) Incidence and surgical importance of Zuckerkandl's tubercle of the thyroid and its relations with recurrent laryngeal nerve. ISRN Surg 2012: 450589.
- Gravante G, Delogu D, Rizzello A, et al. (2007) The Zuckerkandl tubercle. Am J Surg 193: 484-485.
- Serpell JW (2010) New operative surgical concept of two fascial layers enveloping the recurrent laryngeal nerve. Ann Surg Oncol 17: 1628-1636.
- Ching HH, Kahane JB, Foggia MJ, et al. (2018) Medial approach for the resection of goiters with suprahyoid, retropharyngeal, or substernal Extension. World J Surg 42: 1415-1423.
- Randolph GW, Clark OH (2013) Principles in thyroid surgery. In: Randolph GW, Surgery of the thyroid and parathyroid glands. (2nd edn), Elsevier Saunders, Philadelphia, 273-293.
- Beneragama T, Serpell JW (2006) Extralaryngeal bifurcation of the recurrent laryngeal nerve: A common variation. ANZ J Surg 76: 928-931.
- Shao T, Qiu W, Yang W (2016) Anatomic variants of the recurrent laryngeal nerve in Chinese patients: A prospective study of 2,404 patients. Sci Rep 6: 25475.
- Chan WF, Lo CY (2006) Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 30: 806-812.
- Lo CY, Kwok KF, Yuen PW (2000) A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomy. Arch Surg 135: 204-207.
- Serpell JW, Yeung MJ, Grodski S (2009) The motor fibers of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg 249: 648-652.
- Gurleyik E, Cetin F, Dogan S, et al. (2018) Displacement of the recurrent laryngeal nerve in patients with recurrent goiter undergoing redo thyroid surgery. J Thyroid Res 2018: 4763712.
- Wojtczak B, Barczy´nski M (2016) Intermittent neural monitoring of the recurrent laryngeal nerve in surgery for recurrent goiter. Gland Surgery 5: 481-489.
- Jain V (2017) Beahr's triangle: The surgical anatomy world. J Endoc 9: 35.
- Prem Kumar A (2018) The rationale of triangles in relation to thyroid surgery: A proposed unified 'area of danger'' IP Indian Journal of Anatomy and Surgery of Head, Neck and Brain, April-June 4: 48-51.
- Loré JM Jr, Kim DJ, Elias S (1977) Preservation of the laryngeal nerves during total thyroid lobectomy. Ann Otol Rhinol Laryngol 86: 777-788.
- Ekhar VR, Ramkumar V, Shelkar RN, et al. (2018) Identification of external branch of superior laryngeal nerve during thyroid surgery: A prospective study. Int J Otorhinolaryngol Head Neck Surg 4: 228-232.
- Hermann M, Alk G, Roka R, et al. (2002) Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: Effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg 235: 261-268.
- Gimm O, Brauckhoff M, Thanh PN, et al. (2002) An update on thyroid surgery. Eur J Nucl Med Mol Imaging 29: S447-S452.
- Randolph GW (2013) Surgical anatomy and monitoring of the recurrent laryngeal nerve. In: Randolph GW, Surgery of the thyroid and parathyroid glands. (2nd edn), Elsevier Saunders, Philadelphia, 306-340.
- Attie JN, Khafif RA (1975) Preservation of parathyroid glands during total thyroidectomy. Improved technic utilizing microsurgery. Am J Surg 130: 399-404.
- Kandil E, Singer M, Deniwar A, et al. (2016) Surgical approaches to the recurrent laryngeal nerve. In: Randolph GW, The recurrent and superior laryngeal nerve. Springer, Switzerland, 139-144.
Corresponding Author
Dr. Ahmed S. Abdulsamad, Department of General Surgery, Al Zahra Hospital, Dubai, UAE.
Copyright
© 2022 Alarnaout S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.