Pharyngeal Pouch and Concurrent Tongue Base Squamous Cell Carcinoma: An Unusual and Challenging Dual Pathology Causing Dysphagia
Abstract
Dysphagia is a common symptom in patients presenting to physicians in primary and secondary care. The term dysphagia describes the perception of obstruction during swallowing. The initial consideration when dealing with this symptom is to exclude serious pathology such as a malignancy. In this case report, we describe an unusual combination of two pathologies to account for dysphagia in our patient; a synchronous pathology of pharyngeal pouch and a tongue base squamous cell carcinoma. The combination of these two pathologies occurring together is extremely rare and both pathologies can present with dysphagia as the main presenting symptom. We share this case to raise awareness among colleagues, as to the best of our knowledge this has not been reported in the published literature.
Keywords
Otolaryngology, Head and Neck Neoplasms, Pharyngeal Pouch, Dysphagia
Introduction
Dysphagia is a common symptom in patients presenting to specialist services [1,2]. It can affect people of any age; however, it is predominantly found amongst older patients. The term dysphagia is commonly used to describe the perception of obstruction during swallowing. It has a prevalence of nearly 22% in the adult primary care population and 13.5% in the general population [3]. The key initial consideration when dealing with such symptom is to rule out a serious pathology like malignancy causing the dysphagia.
The initial description of dysphagia offers an expansive list of potential causes, however, an organised approach by means of thorough clinical history and use of modern diagnostic techniques can help determine the underlying pathology.
In this case report we describe a very unusual combination of two pathologies to account for dysphagia in our patient. A synchronous pathology of pharyngeal pouch and tongue base squamous cell carcinoma (SCC) is extremely rare and both pathologies can present with dysphagia as the main presenting symptom. We share this case to raise awareness among colleagues, as to the best of our knowledge this has not been reported in the published literature.
Case Report
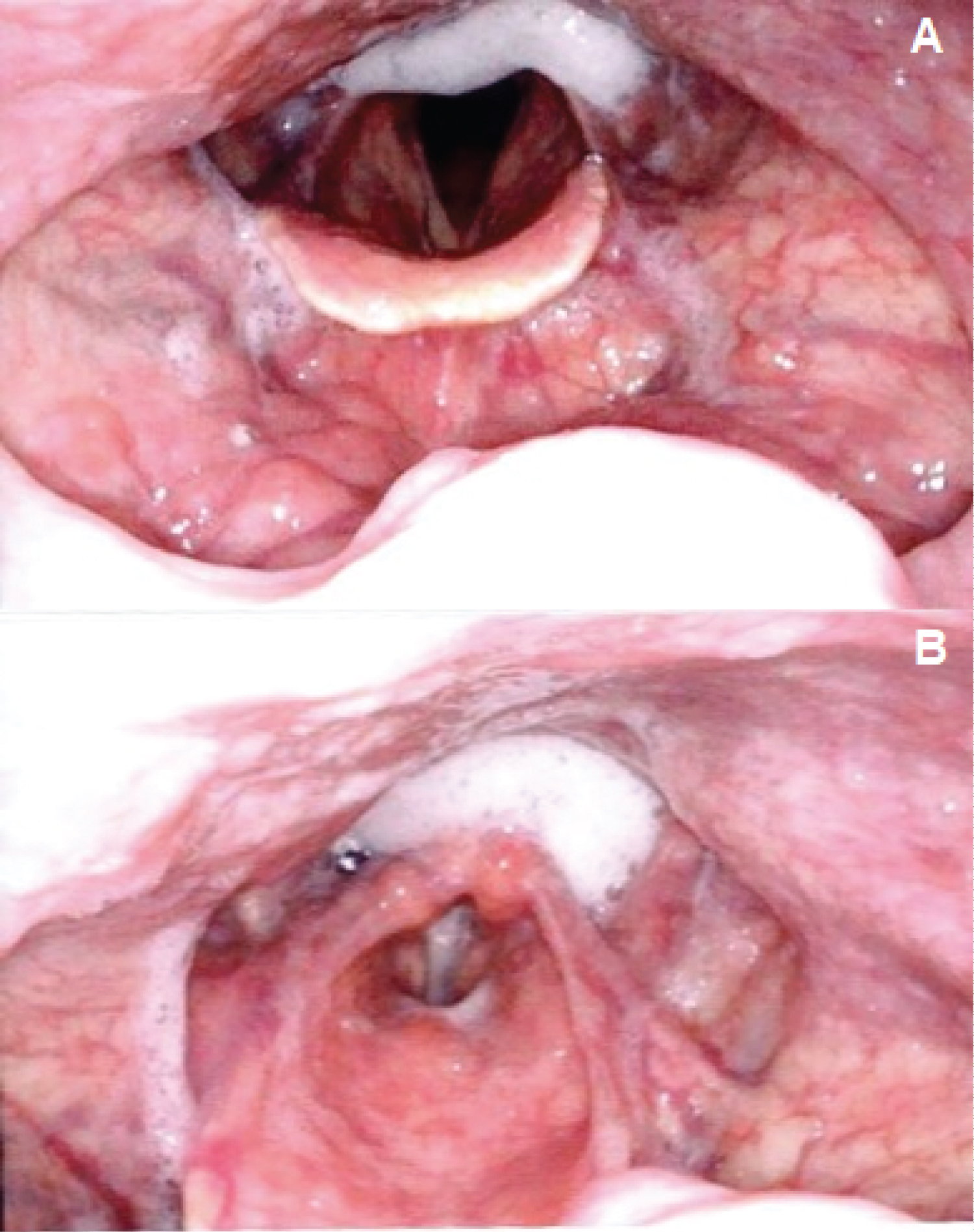
A 69-years-old Caucasian male presented to the ear, nose and throat (ENT) department with a 3-week history of right anterior neck swelling, preceded by an upper respiratory tract infection. Additionally, the patient reported ongoing symptoms of throat irritation, regurgitation of old undigested food, halitosis and progressive dysphagia for solids for the past one year, with some difficulties in swallowing medication tablets as well. No other upper aerodigestive tract red-flag symptoms were documented. The patient's family and social history were unremarkable. The patient was a non-smoker and consumed alcohol within social limits. Clinical examination revealed a gurgling voice quality indicating build-up of secretions. Oropharyngeal examination was unremarkable. Upon examining the neck, a 5 × 4 cm oval shaped right level 2 lump was noted. The skin overlaying this lump was normal. Flexible nasal endoscopy revealed that both vocal cords were mobile with some pooling of saliva in the pyriform fossae (Figure 1).
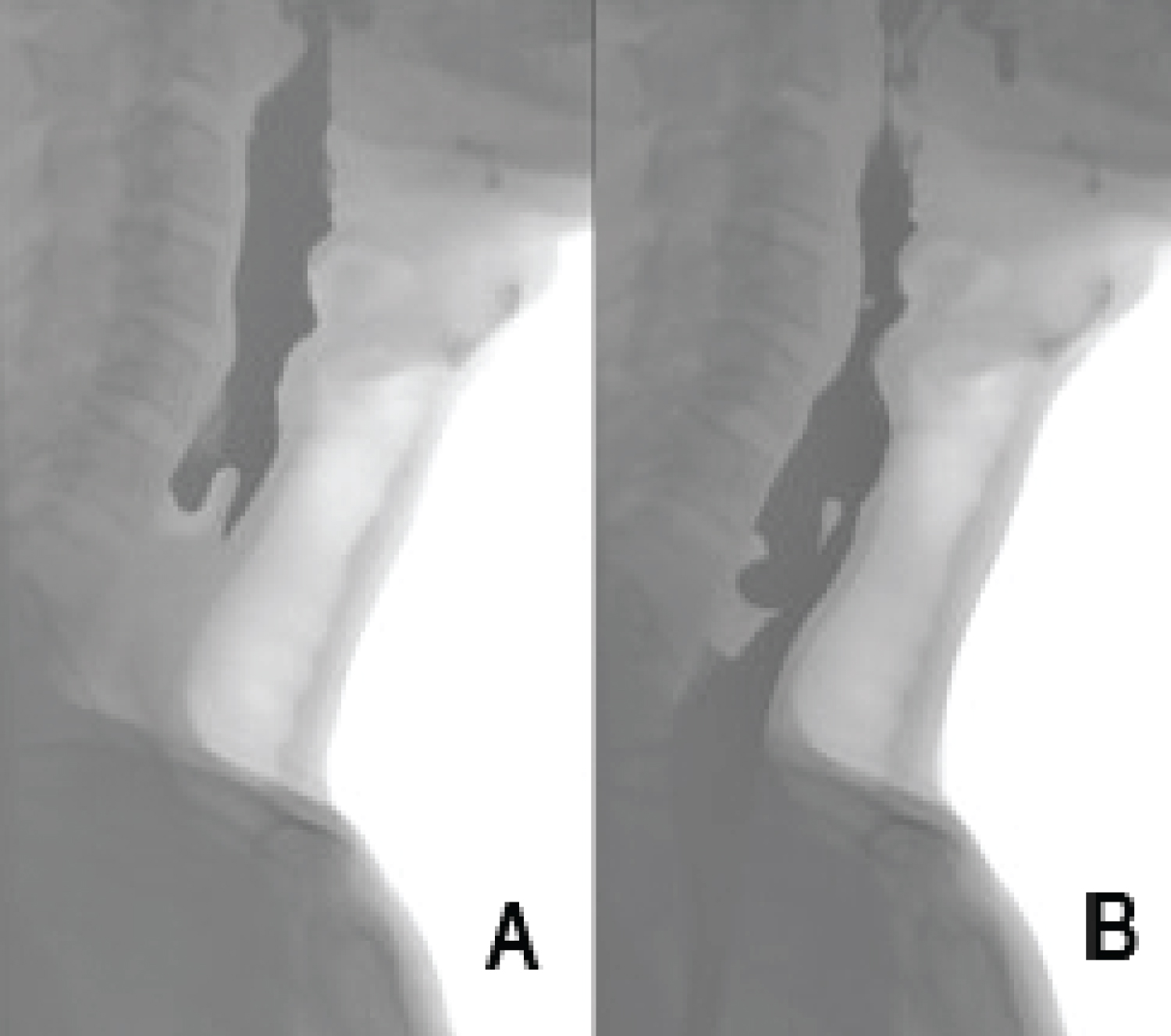
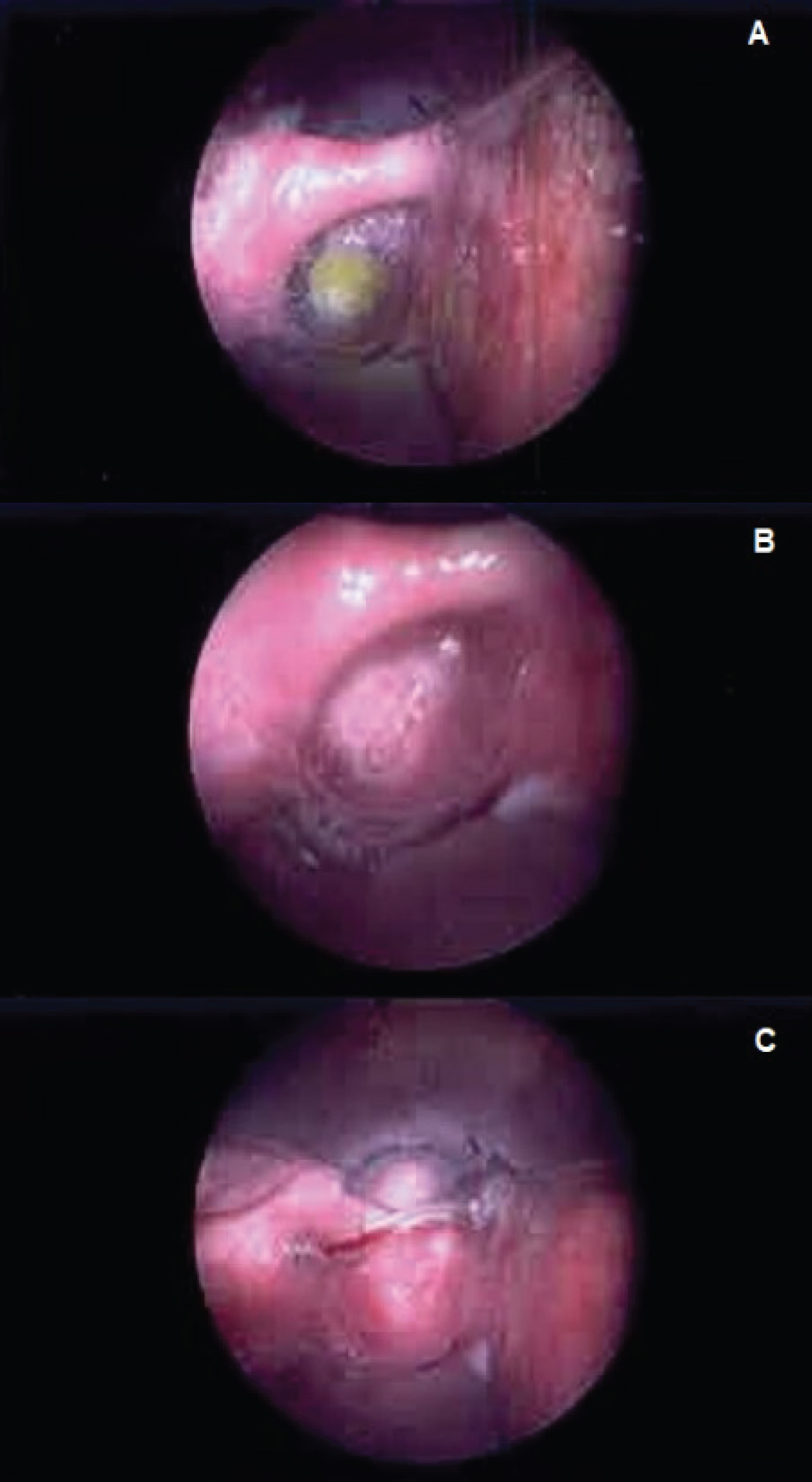
Overall, the patient's history and clinical examination were atypical: Chronic dysphagia and the cardinal symptoms of regurgitation of old undigested food with signs of saliva pooling in the hypopharynx are in keeping with a pharyngeal pouch (Figure 2). A short history of a right neck level 2 neck lump preceded by an upper respiratory tract infection could be attributed to reactive lymphadenopathy, but metastatic cancer remained a possibility. We arranged for a free-hand fine needle aspiration cytology (FNAC) of the neck lump, barium swallow (Figure 2), computed tomography (CT) of the neck and chest (Figure 3), followed by a formal visualisation of the nasopharynx, oropharynx, hypopharynx and glottis under general anaesthetic via panendoscopy (Figure 4). The barium swallow confirmed the diagnosis of a large pharyngeal pouch in our patient, however the cytology report relating to the FNAC was deemed to be non-diagnostic. Because of the possibility of two pathologies co-existing the CT scan of the neck and chest was carried out and to our surprise it raised suspicion of a right hypopharyngeal malignant stricture alongside local pharyngeal dilatation. Following this, the patient underwent a panendoscopy involving a careful examination of the tongue base, pharynx, larynx, hypopharynx, and oesophagus. The pharyngeal pouch was confirmed with a healthy fundus. The right tongue base was noted to have some friable mucosa (Figure 5). The biopsies of this region revealed the additional diagnosis of tongue base SCC. The core biopsy of the recurrent neck lump was carried out after needle aspiration of 10 ml of fluid.
Once it was established intraoperatively that the pharyngeal pouch showed no concerning mucosal lesions, an endoscopic diverticulotomy (stapling) was undertaken using the stapling gun ENDOPATH ETS Articulating Linear Cutter 45 mm (ATS 45) manufactured by Johnson & Johnson's Ethicon. The patient was discussed in our local head and neck multi-disciplinary team meeting. The diagnosis of tongue base cancer was confirmed staged at T1 N1 M0. Chemo-radiotherapy was recommended as the preferred treatment option with a curative intent. Our patient was also a candidate to take part in the DOM-INNATE Trial, which is a randomised clinical trial comparing Duquestide with Placebo as a treatment for oral mucositis. This included two cycles of (Cisplatin 100 mg/m2) accompanied by radiotherapy to the oropharynx and neck, over a 6-week period.
The patient reported complete resolution of his dysphagia, regurgitation and throat irritation after the endoscopic pharyngeal diverticulotomy when reviewed 2 weeks after the procedure. The tongue base SCC was successfully treated with chemo-radiotherapy and the patient is now 3 years post-treatment with no evidence of local or regional disease recurrence.
Discussion
Our review of the literature suggests that this is the first report of synchronous benign pathology pharyngeal pouch and malignant pathology right tongue base poorly differentiated squamous cell carcinoma T1 N1 M0 P16 +ve. A high index of suspicion is required to correctly diagnose a case such as this.
A Pharyngeal pouch can present with a multitude of symptoms, including a foreign body sensation in the throat, recurrent aspiration pneumonia, dysphagia, posterior neck swelling, and regurgitation of undigested food. However, in light of a neck swelling history, progressive dysphagia requires exclusion of malignancy as the underlying cause [4]. In our case the pharyngeal pouch walls and fundus were carefully and thoroughly examined endoscopically to rule out any cancer (Figure 4).
As the symptoms of pharyngeal pouch and tongue base cancer overlap, it is vital to carefully and thoroughly examine the oral cavity and the upper aerodigestive tract of all pharyngeal pouch patients. This will ensure that patients with dual pathology are properly diagnosed and may also provide ENT specialists with the chance to detect tongue base cancers earlier. We recommend direct visualisation in the form of panendoscopy when diagnostic imaging findings are not clear.
Conclusions
Dysphagia can be associated with pharyngeal pouch. Consider the presence of other oral cavity or other upper aerodigestive tract pathology in pharyngeal pouch patients. Although rare, SCC can arise and hide within the pharyngeal pouch. As the symptoms of pharyngeal pouch and tongue base cancer overlap, the oral cavity and upper aerodigestive tract should be thoroughly examined to exclude the presence of more sinister pathology. When radiological image findings of the neck are not clear, the area in question should be directly visualised with a view to carry out biopsy.
Conflict of Interest
None declared.
References
- Morris H (2005) Dysphagia in a general practice population. Nurs Older People 17: 20-23.
- Cho SY, Choung RS, Saito YA, et al. (2015) Prevalence and risk factors for dysphagia: A USA community study. Neurogastroenterol Motil 27: 212-219.
- Wilkins T, Gillies RA, Thomas AM, et al. (2007) The prevalence of dysphagia in primary care patients: A hames net research network study. J Am Board Fam Med 20: 144-150.
- Shakeel M, Sankar V, Vallamkondu V, et al. (2015) Preservation of speech and swallowing after excision of a pharyngeal pouch tumour. J Coll Physician Surg Pak 1: S50-S52.
Corresponding Author
Dr. Muhammad Shakeel, Department of Otolaryngology-Head and Neck Surgery, Aberdeen Royal Infirmary, Ward 210, Aberdeen, AB25 2ZN, United Kingdom, Tel: 00441224552117, Fax: 00441224554569
Copyright
© 2020 Sharma P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.