Vaginal Cuff Dehiscence and Evisceration 40-Years after Abdominal Hysterectomy
Abstract
Vaginal cuff dehiscence is a rare but serious complication of hysterectomy and caries even more risk of morbidity and mortality when evisceration occurs. Vaginal cuff dehiscence can occur at any time after hysterectomy; thus, it is important to identify risk factors in patients and counsel them on signs and symptoms of dehiscence. Once diagnosed, minimally invasive approaches such as vaginal and laparoscopic techniques should be the preferred method of repair. We present a case of an 85-year-old woman who presented with abdominal pain and sensation of a bulge in her vagina 40-years after total abdominal hysterectomy. She was diagnosed with vaginal cuff dehiscence and evisceration and underwent complete vaginal repair and colpocleisis.
Keywords
Vaginal cuff dehiscence, Bowel evisceration, Vaginal repair, Colpocleisis
Introduction
Vaginal cuff dehiscence and eviscerations are rare but serious complications of hysterectomy, which are defined as the partial or total separation of the vaginal cuff with protrusion of abdominal and/or pelvic contents into the vagina [1]. The incidence of vaginal cuff dehiscence varies based on the method of hysterectomy with 1-4% occurrence after laparoscopic/robotic approach vs. 0.14-0.27% occurrence with vaginal and open abdominal approach [2,3]. The even rarer subset of this complication, evisceration through the vaginal cuff, occurs approximately 0.03-1.2% of the time and can include pelvic and abdominal organs such as the small bowel, omentum, fallopian tubes, and/or appendix [1-3].
Although the occurrence is rare, the morbidity and mortality of this complication is high secondary to potential bowel strangulation, incarceration, necrosis, and/or perforation [4]. There is also risk for vaginal bacteria to enter the peritoneal cavity leading to peritonitis and sepsis [4]. Risk factors for vaginal cuff dehiscence include postmenopausal status, multiparity, early resumption of sexual activity post-hysterectomy, factors associated with poor wound healing (including malignancy, chronic steroid use, malnutrition, tissue radiation, immunocompromise, and diabetes mellitus), repetitive Valsalva Maneuver (chronic cough), and postoperative vaginal cuff infection or hematoma [2,5,6]. The following describes an interesting case of vaginal cuff dehiscence and evisceration as it took place greater than 40-years after hysterectomy was performed.
Case
The patient is an 85-year-old woman, gravida 5, para 3, with a significant past medical history of coronary artery disease, hypertension, and hyperlipidemia. Her past surgical history is significant for total abdominal hysterectomy performed in 1980 for unknown etiology. She presented to an outside hospital with complaint of abdominal pain and a mass protruding though her vagina. On presentation, the patient reported she was straining in the bathroom to have a bowel movement and had sudden onset severe abdominal pain and sensation that a mass was protruding into her vagina. On evaluation in the emergency room the patient was diagnosed with a vaginal cuff dehiscence and small bowel evisceration into the vagina. The small bowel was returned through the vagina into the abdominal cavity and vaginal packing was inserted to prevent further protrusion of the bowel. A Foley catheter was also placed at this time. The patient was given Vancomycin 1g and then subsequently started on Piperacillin/Tazobactam 3.375 g q6 h and Metronidazole 500 mg q8 h. The patient had a CT scan of the abdomen and pelvis confirming prolapse of the bowel into the vagina. Preparations were then made to transfer the patient to our facility for further evaluation and surgical management.
Upon arrival, she reported mild abdominal pain that was able to be controlled with intravenous pain medications. The patient denied any previous history of vaginal cuff dehiscence or prolapse of the vaginal cuff since her original surgery in 1980; however, she had not seen a gynecologist in approximately 10-years. She denied any previous problems with urination or defecation. She reports she was last sexually active approximately 5-years ago and did not plan on being sexually active again.
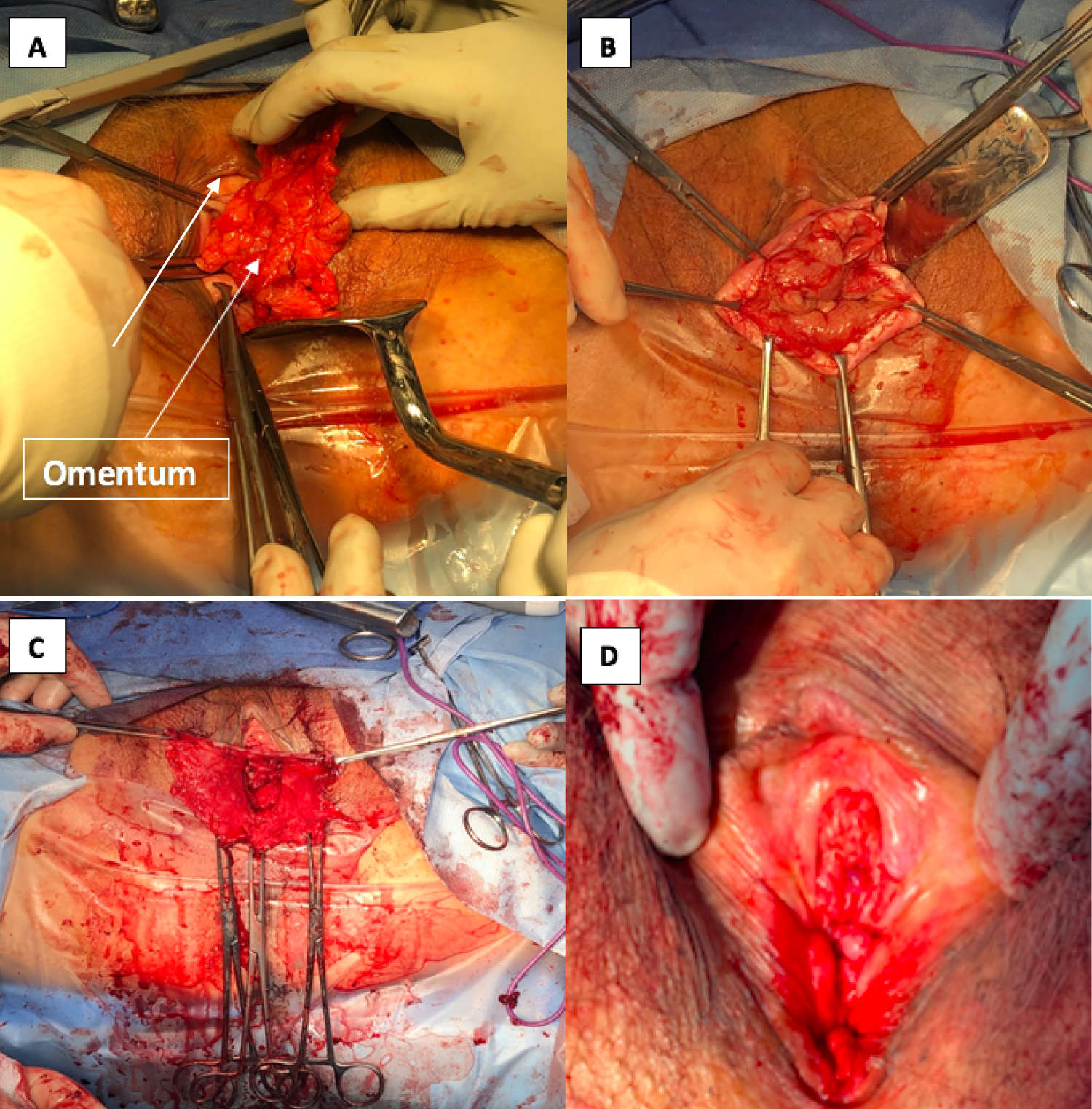
Her vital signs on admission were 98.0 ℉, pulse 60, respiratory rate 18, and blood pressure 186/81. Her WBC on admission was normal, her Hgb was 11.1 g/dl and she had no electrolyte abnormalities. Vaginal packing and Foley catheter were left in place with plans to do exam under anesthesia in the operating room at time of repair. Exam under anesthesia in the operating room revealed epithelialized omentum protruding into the vagina (Figure 1A) and bowel adherent to inner aspect of the vaginal epithelium (Figure 1B). The vaginal cuff opening was measured to be 8.0 × 5.0 cm. The portion of the epithelialized omentum protruding through the vagina was excised. Vaginal epithelium was dissected from the underlying connective tissues in its entirety and excised. Adhesions from the bowel were released. The bowel was examined and noted to be healthy appearing and was replaced through the vagina into the pelvis (Figure 1C). A colpocleisis was then performed in the usual fashion (Figure 1D). Pathology revealed omental adipose tissue with focal acute inflammation and fibrosis and benign squamous mucosa with hyperkeratosis of the vaginal epithelium.
The patient met all her postoperative milestones and was ultimately discharged home in stable condition on post-operative day three. She was seen in the outpatient clinic on post-operative day nine and on exam operative site was intact and healing well.
Discussion
Our patient's case is unusual in that her cuff dehiscence occurred 40-years after her abdominal hysterectomy. In reviewing retrospective cohort studies and case series, Cronin, et al. has shown that the average time to cuff dehiscence was 6.1 weeks to 1.6-years; however, this also differs based on type of hysterectomy. For example, a review of a list-serve of case reports showed that the average time to cuff dehiscence after a total laparoscopic hysterectomy was 7 weeks, meanwhile the average after total abdominal hysterectomy was 13 weeks [3]. In our case, we suspect that this patient's dehiscence was partly due to vaginal atrophy which likely led to a slow and chronic breakdown of her vaginal cuff allowing the progressive protrusion of omentum into the vagina over time. She became symptomatic when this chronic breakdown was finally so weak that complete evisceration occurred secondary to her straining to have a bowel movement. This is not an unusual antecedent evident to cuff dehiscence with the literature reporting common precipitating events to be vaginal intercourse (8-48%), straining with a bowel movement (16-30%), and Valsalva Maneuver [3]. However, many patients report no antecedent event to symptom onset (up to 70%) [3].
As noted previously, this is a serious complication with risk for severe morbidity if left untreated which is why it is important to recognize quickly. Most patients will report within the first 24 hours of symptom onset and the most common chief complaints are pelvic and/or abdominal pain (58-100%), and vaginal bleeding and/or watery vaginal discharge (33-90%) [3]. It is important to know what type of hysterectomy the patient had as one may be more concerned for cuff dehiscence if a patient had a laparoscopic or robotic hysterectomy since there is clear evidence in the literature that this is a greater risk factor. For example, in an observational case series, over 7000 hysterectomies were reviewed and found that total laparoscopic hysterectomy has 21 times the risk compared to total vaginal hysterectomy and 53.2 times the risk compared to total abdominal hysterectomy for cuff dehiscence [7]. Once the diagnosis is made, the method of repair must be decided upon. Repair can be done vaginally, laparoscopically, or abdominally, with preference to the more minimally invasive approaches if possible.
In Cronin, et al. [3] review of the literature, 51% of dehiscence was repaired vaginally, 32% were repaired abdominally, 2% were repaired laparoscopically, 10% were repaired by a combined approach, and 5% were allowed to heal by secondary intention. Traditionally, open abdominal approach has been preferred to assess the integrity of the bowel, however as more cases are reported it appears a minimally invasive approach may also be reasonable [8]. Advantages to vaginal repair include shorter hospital length of stay and shorter postoperative recovery times compared to an open abdominal incision, the obvious disadvantage is the inability to run the bowel and examine other pelvic structures [8]. In our case, we were prepared to enter the abdomen laparoscopically if we thought it necessary. After removing the epithelialized portion of the omentum and freeing the bowel from the adhesions to the vaginal epithelium at the cuff, we were not concerned for any bowel injury and thus did not feel it was necessary to increase operative time and anesthesia exposure for our patient in order to run the bowel. In addition, our patient had no gastrointestinal symptoms and no clinical or lab abnormalities suggesting bowel injury or peritonitis.
Our repair differed from most other cases that are reported in the literature as we performed a colpocleisis as opposed to just repairing the vaginal cuff. In elderly patients who are no longer interested in having vaginal intercourse this is a good option for treatment as it eliminates the possibility of another cuff dehiscence. For patients who still desire the ability to have vaginal intercourse, several other methods of cuff repair after dehiscence have been reported, such as repair with absorbable suture and omental flap, continuous locking stitches with polyglactin, the use of overlying polyglatcin mesh, and multiple figure of eight sutures of polyglactin, [1,2,5]. One case report of dehiscence 17-years after hysterectomy described the repair of the initial dehiscence vaginally with a double layer cuff closure using polyglactin. The patient was then brought back to the operating room 16 weeks later for a laparoscopic Sacro colpopexy with polyprolene mesh for apical support, with hopes that it would decrease recurrence [5].
Efforts should also be made during initial hysterectomy to try and reduce the risk of this unwanted complication. Since we know based on the literature that there seems to be increased risk of cuff dehiscence after laparoscopic and robotic hysterectomies some may believe that these methods are inferior to vaginal or abdominal approaches; however, there are clear advantages to minimally invasive methods of hysterectomy, such as decreased hospitalization time and increased healing time for patients. Thus, it is important to investigate ways to reduce cuff dehiscence after laparoscopic approached to hysterectomy. A retrospective review showed that using bidirectional barbed suture for cuff closure has shown to significantly decrease the rate of vaginal cuff dehiscence over other methods of closure (0% vs. 4.2%, p = 0.008) during laparoscopic and robotic hysterectomies, while not increasing the rate of postoperative bleeding, cuff cellulitis, or granulation tissue formation [9]. It is also possible that since laparoscopic, and robotic hysterectomy are newer techniques, that as surgeons become more adept this complication rate may decrease to match that of vaginal and abdominal approaches.
Patients should also be instructed on ways they can reduce their risk of cuff dehiscence. There is no set guideline of when patients can resume vaginal intercourse; however, most gynecologic surgeons will re-evaluate their patients approximately 6-8 weeks after surgery to assess the integrity and healing of the vaginal cuff. One report by Kahramanoglu, et al. advised that patients should wait at least 8 weeks prior to engaging in vaginal intercourse after hysterectomy [10]. Patients should also be advised about the management of other risk factors such as good diabetic control pre and post-operatively and good nutritional status to support tissue integrity and postoperative healing. Patients can also be advised to use over the counter stool softeners as needed to avoid constipation and straining.
Conclusion
Vaginal cuff dehiscence with evisceration, although rare, is a serious complication of hysterectomy that needs to be diagnosed quickly and managed appropriately to avoid severe morbidity for affected patients. Minimally invasive management with vaginal or laparoscopic approaches are preferred when appropriate. When there is no concern for bowel injury even if there is evisceration, it is safe to manage the case with a vaginal approach as made evident by our case.
Acknowledgment
None.
Disclosures
The authors have nothing to disclose.
Disclosure Statement
All authors declare that they have no conflicts of interest and nothing to disclose.
Ethics Statement
No IRB approval was required to write this case report.
Source of Funding
None.
Statement of Prior Presentation/Publication
This manuscript has not been submitted for prior publication or presentation.
References
- Safta YB, Ghalleb M, Baccari A, et al. (2017) Vaginal cuff dehiscence and evisceration 11 years after a radical hysterectomy: A case report. Int J Surg Case Rep 41: 234-237.
- Jareemit Nida, Chenchit Chayachinda, Nichamon Parkpinyo, et al. (2017) Vaginal Cuff Dehiscence with Small Bowel Evisceration 14 Months after Total Abdominal Hysterectomy. Siriraj Medical Journal. 69: 391-394.
- B Cronin, VW Sung, KA Matteson (2011) Vaginal cuff dehiscence: Risk factors and management. Am J Obstet Gynecol 206: 284-288.
- E Sterk, K Stonewall (2020) Vaginal cuff dehiscence - A potential surgical emergency. American Journal of Emergency Medicine 3.
- Baines G, Jackson SR, Price N (2017) Laparoscopic management of spontaneous vaginal vault dehiscence and bowel evisceration 17 years following total abdominal hysterectomy. Gynecol Surg 14: 1.
- Ramirez PT, Klemer DP (2002) Vaginal evisceration after hysterectomy: A literature review. Obstet Gynecol Surv 57: 462-467.
- Hur Hye-Chun, Richard S Guido, Suketu M Mansuria, et al. (2007) Incidence and Patient Characteristics of Vaginal Cuff Dehiscence after Different Modes of Hysterectomies. Journal of Minimally Invasive Gynecology 14: 311-317.
- Bleull Samantha, Hunter Smith, Robert Shapiro (2017) Transvaginal Management of Vaginal Cuff Dehiscence with Bowel Evisceration Following Delayed Diagnosis. Case Reports in Obstetrics and Gynecology.
- Siedhoff MT, Yunker AC, Steege JF (2011) Decreased incidence of vaginal cuff dehiscence after laparoscopic closure with bidirectional barbed suture. J Minim Invasive Gynecol 18: 218-223.
- V Kahramanoglu Sal, Veysel Sal, T Bese (2016) Post-coital vaginal cuff dehiscence with small bowel evisceration after laparoscopic type II radical hysterectomy: A case report. Int J Surg Case Rep 26: 81-83.
Corresponding Author
Gabriella Pinho, MD, Department of Obstetrics, Gynecology & Women's Health, Rutgers New Jersey Medical School, 185 South Orange Avenue, Medical Science Building, MSB E-506, Newark, NJ 07103, USA.
Copyright
© 2020 Pinho G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.