Assessing Social Determinants of Health among Patients with Depression at Primary Health Care Centers in Riyadh City
Abstract
Background and purpose: Depression is a common and serious medical illness that greatly influenced by socio-economic, demographic, and biological factors. The recognition of social determinants of depression can help reducing the risk factors and promoting mental health. The purpose of this study was to assess the social determinants of patients with depression and to classify its categories at primary health care centers in Riyadh, Saudi Arabia.
Methodology: A cross-sectional study using a self-administered questionnaire was conducted among 322 participants who were selected through convenience sampling technique from June 2021 to August 2022. The study included 18 years of age and older of Saudis and non-Saudis patients at Ministry of Health PHCCs in Riyadh city. Independent samples of t-test and One-Way ANOVA test was used to assess differences in means of numerical variables. Correlations were made by Pearson correlation coefficient. P value of < 0.05 was set as the level of statistical significance. Logistic regression was used to determine the main variables associated with moderate to severe depression.
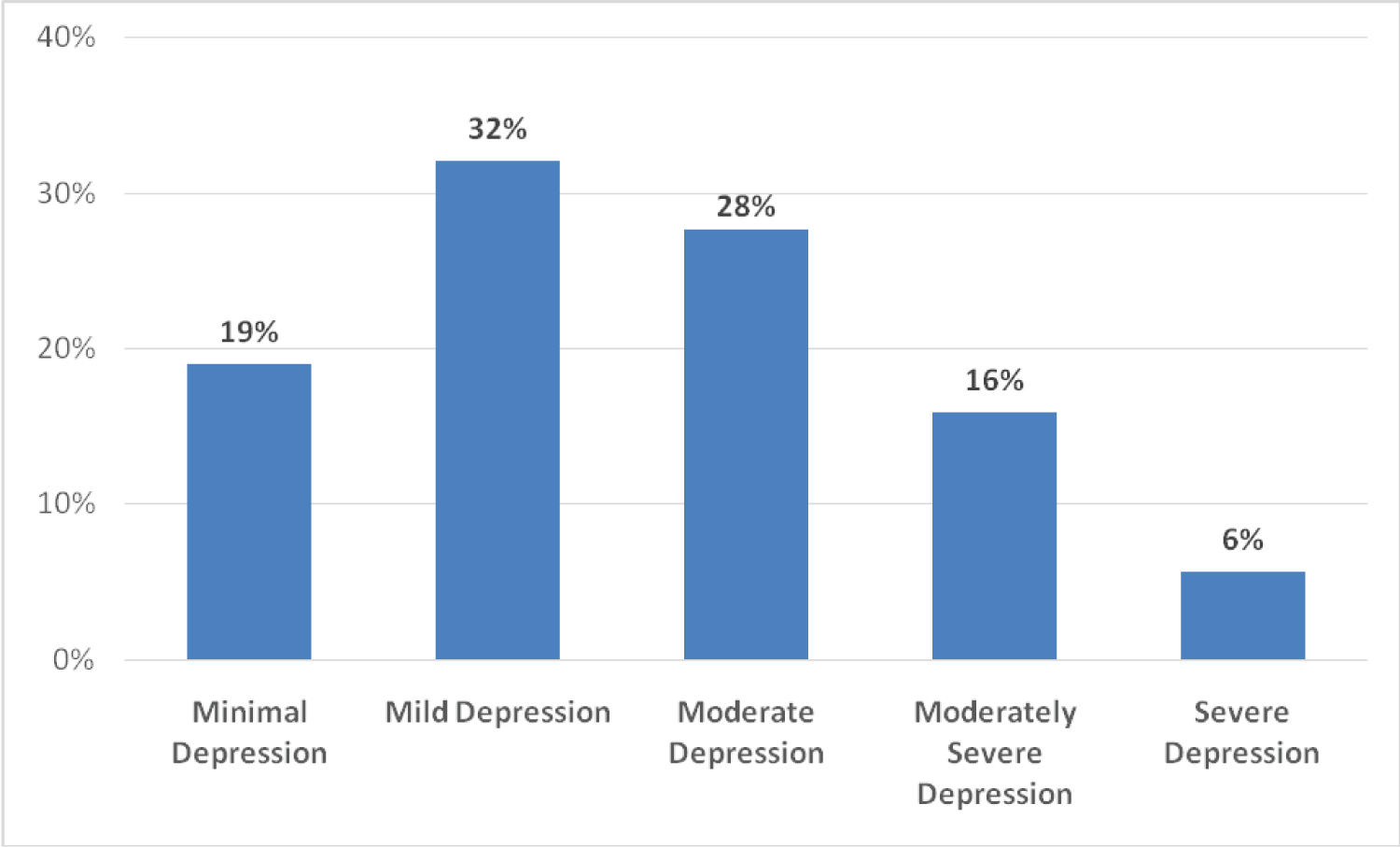
Results: There were (51%) who had minimal to mild depression, (27%) had moderate depression, while (22%) had moderately severe to severe depression. A greater proportion of females had moderate to severe depression (61%) (p = 0.007). Also, moderate to severe depression was higher in those with lower monthly income (54%) (p = 0.03). Saudi nationals were found to have a higher percentage of moderate to severe depression (51%) (p = 0.007). Marital status was found to be associated with depression as single respondents were more likely to have moderate to severe depression (p = 0.052) with 54%.
Conclusion: Social determinants of health including gender, income, marital status, and nationality are associated with depression. Having a comprehensive system focusing not only on the mental health services but also on the social determents of mental health is very important. Future research is needed to understand the association between depression and SDOH in Saudi Arabia. The study results can help policymakers determine the areas that require improvements.
Keywords
Depression, Social, Determinants of health, Saudi Arabia, Primary health care centers
Introduction
Mental health
Mental illness is a significant public health problem which requires attention from people in charge. Mental health disorders are a concern for people of all ages, from early childhood through old age. Many conditions fall under the area of mental illness, including depression, schizophrenia, bipolar disorder, obsessive compulsive disorder, panic disorder, posttraumatic stress disorder, personality disorder, eating disorders, and addictive behaviors. Those kinds of illnesses receive a high public health concern because they affect individuals with different ages, ethnicities, cultures, religions, and incomes. Mental health requires public health interventions such as raising awareness of the importance of mental health, along with establishing mental health screening and treatment services to reduce the burden of the disease [1].
Depression
Depression is defined as the the presence of feelings of sadness, emptiness, or irritability that lasts for a long period of time and has an impact on the functioning of daily life [2]. Symptoms of depression include loss of interest and enjoyment, low energy, and lower activity for at least two weeks. People with depression have also reported anxiety symptoms, disturbed sleep and appetite, and may have feelings of guilt or low self-worth, and difficulty concentrating [3]. Depression is influenced by some factors including genetics, physiology, and psychology [3]. Depression is influenced by social inequalities, income, education, and access to health care as they play a huge role in determining the mental health status [4]. Depression is one of the treatable mental illnesses as studies have shown that 80-90% of people with depression, get treated with a high response to the medication [5].
According to the World Health Organization (WHO), more than 264 million people suffer from depression around the world [6]. According to the Centers for Disease Control and Prevention, depression is estimated to cause 200 million lost workdays each year at a cost to employers worldwide [3]. The WHO has considered depression to be a leading cause of disability around the world and contributes to the global burden of disease. Depression can be long-lasting or recurrent and impacts the quality of life of individuals [6].
In Saudi Arabia, there is a high prevalence of mental health disorders. The prevalence of mental health problems in primary health care centers is 60% [7]. According to a national study that enrolled 477 people, 49.9% of them had depressive symptoms. Depression was higher among females and higher educational level based on the results [8]. In 1983, the Ministry of Health in Saudi Arabia began to provide psychiatric services by developing 21 hospitals with mental health services. Many patients suffering from depression may not seek help from mental health professionals. Therefore, it is very important to screen for mental health at primary health care centers, which could ensure providing physical and mental needs for the patients. According to CDC, depression screening and treatment with psychotherapy and medications are highly suggested since 80% of patients with depression show improvement after treatment [3]. In the United States, about 20% of children and adolescents suffer from mental health disorders during their lifetime. Mental health disorders among children and adolescents can lead to school failure. For U.S adults it is estimated that approximately 17% of adults in the U.S face mental disorders throughout their life [9].
Work productivity is influenced by the status of mental health as people with depression tend to be less productive [3]. A study that focuses on depression in the workplace showed a 6.1% increase in productivity and 22.8% fewer absences over two years for individuals suffering from depression who received regular phone calls to encourage them to continue with depression treatment and medication. Employers saved over $2600 every year for each employee who received guidance on depression management. CDC recommends implementing a health policy that focuses on the worksite lifestyle programs such as physical activity, which could help in both preventing as well as treating depression [3].
COVID-19
Coronavirus disease 2019 (COVID-19) is from the coronavirus family, it first appeared in China in 2019, then it spreads all over the world. The WHO confirmed that it was a global pandemic in March 2020. Symptoms of COVID-19 include fever, dry cough, shortness of breath, tiredness, headaches and altered taste and smell sensation [10]. The government of Saudi Arabia applied public health measures such as enforcing lockdowns, social distancing, shifting work schedules online, and closing malls and restaurants to limit the spread of the COVID-19. The public health measures affected the daily routine of individuals such as physical activities, jobs, and financial situations [11].
Stigma
Depression stigma has been considered a global problem around the world. According to the Mental Health Foundation, nine out of ten people with depression say that social stigma and discrimination have affected their lives throughout their recovery phase [12]. Local and global public health interventions have taken place which mostly aims to raise awareness to limit the stigma associated with depression and improve the health status of people with depression to ensure they have a healthy life [2].
Social determinants of health
Social determinants of health are defined by the CDC, as the conditions in the places where individuals learn, work, play, and live, which affect the health of people [2]. Following are examples of the social determinants of health, that have a great impact on our health in positive and negative ways: “income and social protection, education, unemployment and job security, working life conditions, food insecurity, housing, basic amenities and the environment, early childhood development, social support and inclusion, structural conflict and access to affordable health services [13].
According to the WHO, researchers who are interested in the social determinants of health concluded that the social determinants can be in some cases more important than health care or lifestyles when it comes to impacting health. Several studies suggest that social determinants of health account for almost 50% of health outcomes [13]. SDOH do not only affect physical health but also mental health. Researchers have found a link between SDOH and mental health, social determinants of health have a significant impact on mental health. Stakeholders including Ministry of Health have established policies to focus on treating the social inequalities and social inequities. Social policies will improve the social life of individuals and that will play a role in reducing the burden of mental health illness. Recommended policies by the WHO include the policies to reduce poverty and racial segregation as well as promoting education, healthier homes, neighborhoods, schools and workplaces. Studies have agreed with the findings that low economic status, unemployment, family relationships struggle, and unsafe neighborhoods can play very important role in affecting the mental health of individuals [14].
Mental health/depression health services in Saudi Arabia
As part of the Vision 2030 of Saudi Arabia, the Ministry of Health (MOH) started to develop a new comprehensive healthcare system that covers the health of people socially, mentally, and physically by a new patient‐centered Model of Care [15]. This new model aims to ensure that the services meet the needs the patients seek. The Chronic Care administration at the Ministry of Health spends efforts on mental health. As part of the vision 2030 plan, stakeholders developed a national mental health strategy that ensures the integration of health care services [15]. Such a strategy will help in addressing the gaps in the health care system as well as providing services that cover the quality, accessibility, and integration of care.
The ministry of health in Saudi Arabia established the primary mental health program in 2016 to screen people for the most common mental health illnesses including depression and anxiety [16]. The integration of mental health services in primary health care settings increases the opportunity of screening and treating more people within the community. The MOH provides primary mental health services in over 1000 primary health care centers throughout the regions of Saudi Arabia [15].
This study focuses on the association between depression and social determinants of health in the city of Riyadh, Saudi Arabia.
Purpose
To determine the social determinants of depression in patients at selected Primary Health Care Centers in Riyadh.
Research question
What are the social determinants of depression among patients at primary health care centers in Riyadh city?
Objective of the study
The objective of this study was to determine the social determinants of health for depression among patients visiting primary health care centers in Riyadh city.
Significance of the study
It is very important to determine the SDOH that put individuals at a higher risk of having depression in order to reduce the prevalence of depression by controlling the social determinants of depression. There are limited studies about social determinants of health in Saudi Arabia therefore, it is very important to conduct a study that focuses on social determinants of depression. The SDOH of this study includes age, income, access to health care, marital status, and living condition. To our knowledge, there are limited peer-reviewed studies about social determents of health among depression patients at PHCS in Saudi Arabia. This study will add new information to the current literature about the social determinants of mental health in Saudi Arabia.
Materials and Methods
Setting and design
This is a cross sectional study carried out in 30 primary health care centers in Riyadh city, Saudi Arabia from June 2021 to August 2021.
Subjects
The 322 patients enrolled in the study were PHCs patients at 18 years of age and older including Saudis and non-Saudis.
Target population: Primary health care center visitors in Riyadh-Saudi Arabia. Estimated population of 8.4 million adults.
Sample size: 384
Convenience sampling: It was used, with confidence levels of 95 and 5 percent confidence intervals.
Inclusion criteria: 18 years of age and older. Participants must be a Ministry of Health PHCCs patients in Riyadh city. Saudis and non-Saudis PHCCs patients.
Exclusion criteria: Patients less than 18 years old. Not a Ministry of Health PHCCS patient.
Data collection
Data collection has taken place between June 2021 and August 2021 and was collected through anonymous questionnaire and no personal information was revealed at any circumstances and the participation was voluntary.
The questionnaire consisted of two parts, the demographic questions which included 8 questions followed by both Arabic and English versions of PHQ-9 which has nine questions related to depression. The questionnaire was distributed in a paper form in the chosen PHCCs across the city of Riyadh. The PHCCS the data collected from were located in different regions of Riyadh city, including North of Riyadh, South of Riyadh, West and east of Riyadh, and the center of Riyadh city. The questionnaire was filled by the healthcare provider at the PHCs by asking the patients the assigned questions to ensure complete answer of all questions.
First section included demographic questions; Age, Gender, Income, Marital status, and educational level.
Second section included the PHQ-9, Patient Health Questionnaire. The PHQ-9 is used by primary care physicians, and consists of nine items depression scale of the patient health questionnaire. The nine items are designed based on the diagnostic criteria for major depressive disorder. The Patient Health Questionnaire can be used as a screening tool, and help in diagnosis along with symptom tracking tool that can help track the severity of patient's overall depression and can determine the improvement of specific symptoms with treatment [17].
The PHQ-9 tool is validated and reliable according to studies. The validity of the 9-item PHQ-9 was determined in studies that conducted in 8 primary care and 7 obstetrical clinics . PHQ-9 scores > 10 had a sensitivity of 88% and a specificity of 88% for Major Depressive Disorder. Reliability and validity of the questionnaire have showed psychometric properties.
It is a simple, rapid, effective, and reliable tool for screening and evaluation of the severity of depression among primary health care visitors. The PHQ-9 scoring measures are as the following:
Minimal depression, Total Score: 0-4
Mild depression, Total Score: 5-9
Moderate depression, Total Score: 10-14
Moderately severe, Total Score: 15-19
Severe, Total score: 20-27
Data analysis and management
Data entered and analyzed using Microsoft Excel 365 and IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N.Y., USA).
Both descriptive and inferential statistical analyses were applied. For categorical variables, numbers and percentage were used for expression, for numerical variables, median, mean and standard deviation were employed. Independent samples t-test and One-Way ANOVA test were used to assess differences in means of numerical and categorical variables. Correlations were made by Pearson correlation coefficient. P value of < 0.05 was set as the level of statistical significance.
Results
There were a total of 322 respondents included in the study. These included 230 (71%) males, most of them i.e. 173 (54%) were aged 25 to 34 years and another 89 (28%) were aged 18 to 24 years, and 222 (69%) were single as shown in Table 1. There were 166 (52%) who had graduate degree another 32 (10%) had a postgraduate degree, 206 (64%) were employed while 78 (24%) were students. The monthly income of the majority i.e. 194 (60%) was up to SR 10,000 (US$ 2660) and almost all i.e. 299, 93% were Saudi nationals. There were 164 (51%) who had minimal to mild depression, another 89 (28%) had moderate depression, while 69 (22%) had moderately severe to severe depression as shown in Figure 1.
The depression categories according to the PHQ-9 Questionnaire were categorized into two groups: Minimal/Mild depression (n = 164) and Moderate to Severe depression (n = 158). These were compared by the demographic variables as shown in Table 2. It was seen that a greater proportion of females (61%) had moderate to severe depression as compared to 44% of males (p = 0.007). Also, moderate to severe depression was higher in those with monthly income of less than 10,000 SR (54%) as compared to 32% in those with income > SR 15,000 (p = 0.03). Saudi nationals were found to have a higher (51%) percentage of moderate to severe depression as compared to Non-Saudis in whom it was 22% (p = 0.007). Marital status was found to have a borderline significant association (p = 0.052) with 54% of the single respondents having moderate to severe depression as compared to (39%) of the married respondents. There was no significant association found between the depression category and age group (p = 0.31), education level (p = 0.81), employment status (p = 0.23), and residence status (p = 0.13).
Table 3 shows the results of the logistic regression to determine the main variables associated with moderate to severe depression. All the variables found to be significantly associated with moderated to severe depression (gender, income, nationality) as well as marital status and residence status were included in the logistic regression. The results showed that being female had an adjusted odds ratio (aOR) of 2.30 (95% CI 1.32, 4.00; p = 0.003) as compared to males. Respondents who were single were found to have an aOR of 1.80 (95% CI 1.004, 3.21; p = 0.048) as compared to married respondents. Those with income less than 10,000 SR had an aOR of 2.18 (95% CI 1.06, 4.46; p = 0.03) as compared to those with income greater than SR 15,000. Saudi nationals were found to have an aOR of 3.28 (95% CI 1.10, 9.75; p = 0.03) as compared to Non-Saudis.
Discussion
Depression
To the best of our knowledge, this is the first study in Riyadh city, Saudi Arabia to examine the relationship between depression and social determinants and lifestyle factors in primary health care centers. Depression has been one of the most common mental health conditions worldwide and has been one of the main causes of disabilities [6]. Public health interventions that address depression in Saudi Arabia have been established by the ministry of health including raising the awareness of depression and mental health in general as well as early detection of depression conditions among Primary health care centers visitors. The study concluded that there is an association between depression and gender, income, living condition and marital status. Our results are consistent with a previous published study as depression is associated with social changes. It is possible that changes that occur in people’s life such as (retirement, increased isolation, the death of loved ones, financial struggle and other cultural differences) could contribute to increased depression prevalence. According to Alkhthami's research that took place in the Eastern region of Saudi Arabia, there is a high prevalence of depression among primary health care patients in Saudi Arabia. The prevalence of mental health problems including depression and anxiety in primary health care centers is 60% [7]. Depression is a multifactorial condition that is impacted by biological and environmental factors. This study focuses on a number of factors including gender, age, employment status, income, marital status, educational status and nationality.
Gender
Our study showed that females are more likely to have depression compared to males. A systematic review was conducted in Canada focused on gender and mental health agreed with our conclusion that women are more likely to suffer from depression compared to their male counterparts [18]. Females go through hormonal changes, along with the stress of pregnancy for some women, which can increase the likelihood of developing mental health disorders such as depression. Another study conducted in the Kingdom of Saudi Arabia among Jazan university students has also indicated that gender plays a role as a risk factor for depression as females had a higher mean score for depression compared to males with P-values < 0.05 for all [19]. In contrast, a cross-sectional study conducted in KSA showed that men were more likely to develop depression compared to females with P-values < 0.001. This could be because there were fewer men who participated in the study as the female to male ratio was 2:1 [20].
Age
According to our results, there was no significant association between the depression category and the age groups (p = 0.31). Another study focused on mental health during the COVID-19 pandemic and lockdown concluded that younger adults (< 35 years) p-values < 0.05) were more likely to suffer from mental health compared to other age groups, this could be linked to the fact that younger adults are used to practice their daily life in a certain routine such as going to work or school, driving their cars or riding a train, walking (etc..). The fact that the lockdown prevented them from living their daily lives as they were used to can be behind the increase in the likelihood of developing mental health disorders [21]. Another important finding of a Portuguese study is that the age group of 40-64 years was more likely to suffer from depression compared to other age groups. This could be because this age group has more responsibilities than other age groups such as being in charge of taking care of their kids and work [22,23].
Employment status
According to our results, there was no significant association between the depression category and employment status (p = 0.23). That might be due to the fact that there was a diversity in the age group of the study participants as there were students, workers and unemployed enrolled in the study. In support of our results, a study conducted in Mexico concluded that employment status is not associated with the presence of depressive symptoms in women [24]. In contrast, A study took a place in Canada focused on social determinants of mental showed that being unemployed impacts the health of individuals, including mental health. The link between unemployment and depression could be because of the financial struggle unemployed individuals go through as financial struggle can impact someone’s mental health [25]. A systemic review focuses on depression and employment status worldwide concluded that unemployment can lead to a higher prevalence of depressive symptoms and major depressive disorder [26]. Supporting this result a study was conducted to measure the association between depression and employment status among caregivers, and the results concluded that nonworking caregivers were more likely to suffer from depression compared to working caregivers [27].
Nationality
Saudi nationals were found to have a higher (51%) percentage of moderate to severe depression as compared to Non-Saudis whose it was 22% (p = 0.007). This could be because most of the participants in our study were Saudi.
Monthly income
Our results showed that severe depression was higher in those with a monthly income of less than 10,000 SR (54%) as compared to 32% in those with income > SR 15,000 (p = 0.03). We believed that this could be due to the financial obstacles individuals go through which could increase the likelihood of developing depression compared to those who are financially stable. Financial struggle is very common among university students. A cross-sectional study in Jordan included 1582 undergraduate students concluded that students’ income tends to be a risk factor of anxiety and depression [28]. Similar results were shown by another study among public university students. The study suggests that there is psychological distress among students from lower socioeconomic groups living in the U.S during the COVID-19 pandemic [29].
A study conducted in Thailand to address the financial burden during COVID-19 supports this result as the study determined that there was an association between economic burden, especially self-reported financial problems, and adverse mental health outcomes [30]. According to a systematic review study including 64 studies, low and middle-income communities have been linked to depression. The study focused on antenatal depression [31].
Educational level
There was no significant association between depression and education level (p = 0.81). A study focuses on factors affecting depression during pregnancy showed different results. The study concluded that factors such as the educational level of pregnant women play an important role in the severity of depression [32]. Education makes people more aware of the things that trigger their mental health condition therefore, they could avoid the triggers and have better control over their mental health journey compared to those who are less educated about their health [33]. On the other hand, a study focuses on depression among hospitalized patients with chronic conditions showed that mental health distress was higher among educated patients, this could be since educated patients are more familiar with their health condition and more knowledgeable about the complications of their condition [33].
Marital status
Marital status was found to be one of the risk factors for depression, especially among those who are singles [34]. Our study results showed a significant association (p = 0.052) with 54% of the single participants suffering from depression as compared to 39% of the married participants. This could be due to the loneliness the single individuals feel along with the lack of emotional support that some married people have. Moreover, a study conducted in Taiwan revealed that being divorced can put people at a higher risk of suffering from depression. Divorce is a sensitive matter for many people and it can be very frustrating, especially for those who rely emotionally on their partners [35]. In support of this statement, a study conducted among women in Lukali Nanganda agreed that there was a significant difference between marital status and depression [35]. A study focusing on marital status and depression concluded that separated/divorced/widowed/never-married middle-aged and elderly individuals might be at a high risk of facing depression during their lifetime [36]. In conclusion, individuals with unstable marital statuses are more likely to be depressed. In particular, unstable marital status could lead to financial decline which could result in raising the chance of developing depression [35].
Living condition
Our study results have shown that there was no significant association between the depression category and residence status (p = 0.13). This can be supported by the results of another study conducted on depression and sociodemographic factors. The study results showed that depression is not linked to the living conditions of individuals. In contrast, another study conducted among university students in Saudi Arabia stated that depression is strongly associated with the living conditions of the students as students who live alone reported a higher prevalence of depression [19]. This could be due to missing the support of housemates, especially during academic pressure. In support of this, a study took a place among college students living at poor conditions concluded that depression and anxiety are more common among college students living in a poor area compared to those who live in better areas [37]. Another research conducted on the association between depressive mood and living condition has shown that poor housing quality, noise and air pollution could put individuals living in such an environment at higher risk of facing depressive mood [14]. Living conditions and environmental pollution are risk factors of depression and must be taken into account during planning to prevent depression [14].
Strengths and Limitation
Strengths
The study was conducted among Ministry of health Primary health care patients. This is the first study our knowledge that focuses on depression and social determinants of health among Primary health care centers patients in Riyadh City. This study is novel as it will add new information to the current literature about depression and SDOH.
Limitations
Since this research was conducted among primary health care centers patients only, we were required to distribute the questionnaire among the primary health care centers that provide mental health service. Limited time of data collection along with the fact that not all PHCs provide mental health services made our journey more challenging. The cross-sectional nature of the study limits any causal inferences. The PHQ-9 is not considered a diagnostic tool of depression. Since the sample was conducted among PHC at the ministry of health, all private clinics were excluded hence the results cannot be generalized to the general population. This study was conducted during COVID-19. It could have had an impact on the study population causing unforeseen bias since COVID-19 can affect someone’s mental health status causing instability.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained from institutional review board (IRB) of Ministry of Health Standing committee
IRB number (IRB-20116).
All methods were carried out in accordance with relevant guidelines and regulations.
In the first part of the questionnaire an Informed consent was obtained from all the study Participants.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Competing interests
All authors declare no competing interest.
Funding
Not applicable.
Authors' contributions
PI: Abdulrahman Alqahtani: Contributing in all parts of the study.
Co auther: Noara Alhusseini: Contributing in providing the proper advice and guiding when needed in all parts of the study.
Acknowledgements
Whoever does not thank people has not thanked Allah”. Prophet Mohammed PBUH.
First of all, I would like to praise ALLAH for giving me the opportunity, ambition, and strength to do my master’s degree.
I would like to thank my Thesis advisor Dr. Noara Alhusseini for her great thoughtfulness and efforts along my academic journey as well as the committee members who are here with us today.
I wish to express my deep thank to my employer the Ministry of Health, who gave me this opportunity to complete my master’s degree in this important branch of science and I wish to give my best to serve my country and religion.
I would like to thank my manager Dr. Shaker Alomary for his guidance and support which helped me to achieve my professional goals, and for that I am forever grateful.
References
- Alegría M, Frank RG, Hansen HB, et al. (2021) Transforming mental health and addiction services. Health Affairs 40: 226-234.
- CDC (2020) Depression.
- CDC (2016) Policies | Depression interventions.
- NCMH (2022) National Center of Mental Health.
- APA (2020) Depression.
- WHO (2020) Depression.
- Alkhathami AD, Alamin MA, Alqahtani AM, et al. (2017) Depression and anxiety among hypertensive and diabetic primary health care patients: Could patients’ perception of their diseases control be used as a screening tool? Saudi Medical Journal 38: 621-628.
- Al-Qadhi W, ur Rahman S, Ferwana MS, et al. (2014) Adult depression screening in Saudi primary care: Prevalence, instrument and cost. BMC Psychiatry 14: 190.
- Healthy people 2020 (2020) Social determinants of health.
- Hassan SA, Sheikh FN, Jamal S, et al. (2020) Coronavirus (COVID-19): A review of clinical features, diagnosis, and treatment. Cureus 12: e7355.
- AlHusseini N, Sajid M, Altayeb A, et al. (2021) Depression and obsessive-compulsive disorders amid the COVID-19 pandemic in Saudi Arabia. Cureus 13: e12978.
- Mental health Foundation (2015) Fundamental Facts About Mental Health 2015.
- WHO (2022) Social determinants of health.
- Rautio N, Filatova S, Lehtiniemi H, et al. (2017) Living environment and its relationship to depressive mood: A systematic review. Int J Soc Psychiatry 64: 92-103.
- MOH (2022) MOH and psychatric patients.
- MOH (2021) Comprehensive Health Guidance Initiative - Primary Mental Care Program.
- Sun Y, Fu Z, Bo Q, et al. (2020) The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry 20: 474.
- Eid RS, Gobinath AR, Galea LAM (2019) Sex differences in depression: Insights from clinical and preclinical studies. Progress in Neurobiology 176: 86-102.
- Alharbi H, Almalki A, Alabdan F, et al. (2018) Depression among medical students in saudi medical colleges: A cross-sectional study. Adv Med Educ Prac 9: 887-891.
- AlSaeed S, Alkhawajah N M, Ayyash M, et al. (2022) Assessment of factors associated with depression and anxiety among pwMS in Saudi Arabia. BMC Neurology 22: 120.
- Pieh C, Budimir S, Probst T (2020) Corrigendum to “The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria”. Journal of Psychosomatic Research 139: 110278.
- Cuschieri S, Cuschieri S, China J, et al. (2020) Social determinants of depression: Association with age, gender and primary health care model. European Journal of Public Health 30.
- Pan L, Li L, Peng H, et al. (2022) Association of depressive symptoms with marital status among the middle-aged and elderly in Rural China-Serial mediating effects of sleep time, pain and life satisfaction. Journal of Affective Disorders 303: 52-57.
- Fernández-Niño JA, Bonilla-Tinoco LJ, Astudillo-García CI, et al. (2018) Association between the employment status and the presence of depressive symptoms in men and women in Mexico. Cad Saude Publica 34.
- Kim W, Chen YL (2011) The social determinants of depression in elderly Korean immigrants in Canada: Does acculturation matter? International Journal of Aging and Human Developmen 73: 283-298.
- Amiri S (2021) Unemployment associated with major depression disorder and depressive symptoms: A systematic review and meta-analysis. International Journal of Occupational Safety and Ergonomics 28: 1-43.
- O’Neill A, Gallagher S, Hannigan A, et al. (2022) Association between work status and depression in informal caregivers: A collaborative modelling approach. European Journal of Public Health 32: 59-65.
- Naser AY, Alwafi H, Amara NA, et al. (2021) Epidemiology of depression and anxiety among undergraduate students. International Journal of Clinical Practice 75.
- Browning MHEM, Larson LR, Sharaievska I, et al. (2021) Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS One 16:
- Ruengorn C, Awiphan R, Wongpakaran N, et al. (2021) Association of job loss, income loss, and financial burden with adverse mental health outcomes during coronavirus disease 2019 pandemic in Thailand: A nationwide cross-sectional study. Depression and Anxiety 38: 648-660.
- Dadi AF, Miller ER, Mwanri L (2020) Antenatal depression and its association with adverse birth outcomes in low and middle income countries: A systematic review and meta-analysis. PLoS One 15: e0227323.
- Aktas S, Calik KY (2015) Factors affecting depression during pregnancy and the correlation between social support and pregnancy depression. Iran Red Crescent Med J 17: e16640.
- Fattouh N, Hallit S, Salameh P, et al. (2019) Prevalence and factors affecting the level of depression, anxiety, and stress in hospitalized patients with a chronic disease. Perspect Psychiatr Care 55: 592-599.
- Yan X-Y, Huang S-M, Huang C-Q, et al. (2011) Marital status and risk for late life depression: A Meta-analysis of the Published Literature. Int J Med Res 39: 1142-1154.
- Huang F-Y, Li M (2019) The relationship between marital status, cohort, and depression symptoms in Taiwan. Innov Aging 3: S311-S312.
- Bjørnnes AK, Parry M, Lie I, et al. (2018) The association between hope, marital status, depression and persistent pain in men and women following cardiac surgery. BMC Womens Health 18: 2.
- Marthoenis, Meutia I, Fathiariani L, et al. (2018) Prevalence of depression and anxiety among college students living in a disaster-prone region. Alexandria Journal of Medicine 54: 337-340.
Corresponding Author
Abdulrahman Abdullah Alqahtani, Consultant Psychiatrist, Mental Health Department, Federal Teaching Hospital, Ido-Ekiti; Lecturer, Department Of Mental Health, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria, Tel: +234-805627-9692.
Copyright
© 2023 Abdulrahman Abdullah Alqahtani. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.