Interdisciplinary Innovation: Applying the Silfverskiöld Technique to Peri-Areolar Mastopexy-Augmentation Closure
Abstract
Introduction: Among the array of mastopexy techniques, the peri-areolar approach offers minimal scarring and effective repositioning, ideal for mild to moderate ptosis. However, challenges in maintaining optimal nipple-areolar complex (NAC) positioning persist, exacerbated when combined with implants. This study explores the adaptation of the Silfverskiöld technique, known for its tension distribution and repair stability in tendon injuries, to peri-areolar mastopexy-augmentation closure.
Methods: This retrospective case series examined outcomes of breast augmentation and peri-areolar mastopexy employing the Silfverskiöld technique for NAC closure in patients with grade 1 ptosis. Key surgical steps include a doughnut-shaped incision, de-epithelisation, dermal shelf creation, purse-string suture, subcutaneous closure, and Silfverskiöld closure. Outcome measures included NAC diameter at surgery, 3 months, and 1-year post-operation, patient satisfaction, and complications.
Results: Seven female participants (mean age: 39.4 years) were followed for a minimum of 12 months. The mean implant size was 359.29 cc, with varied pocket techniques and implant types. Immediate post-surgery, the median NAC diameter was 42.00 mm. At 3 months, it remained consistent at 42.00 mm, with a slight increase to 43.00 mm at 12 months. Statistical analysis revealed a significant yet clinically acceptable change. Implant size and pocket technique showed no significant influence on NAC diameter at 12 months. There were no complications, and patients expressed high satisfaction.
Conclusion: The adaptation of the Silfverskiöld technique to peri-areolar mastopexy-augmentation closure offers promise in minimizing NAC distortion and maintaining stable outcomes. Further research and refinement hold potential for enhancing the procedure's aesthetic quality and longevity.
Introduction
In the ever-evolving speciality of plastic and reconstructive surgery, the dynamic intersectionality between distinct surgical domains often becomes a catalyst for innovative procedural advancements. Breast augmentation and mastopexy, once secluded in their individual developmental trajectories, have in contemporary practice, converged into a sophisticated amalgam, addressing not merely volumetric enhancement but also, meticulously considering the aesthetic and anatomical recalibration of the breast mound. Within this arena, an array of mastopexy techniques, each meticulously tailored to diverse patient-specific needs and aesthetic aspirations, have found their niche. Yet, even amidst the refinement of these techniques, challenges, particularly pertaining to the delicate art of achieving and maintaining ideal nipple-areolar complex (NAC) positioning and morphology, linger palpably in surgical outcomes and longevity of results.
Navigating through the panorama of mastopexy strategies, the peri-areolar technique has established itself as a modality offering minimal scarring with subtle yet effective repositioning and reshaping capabilities, particularly apt for mild to moderate ptosis and concomitant areolar modifications. Despite its merit, inherent in its application, is the perpetual battle against post-operative areolar distortion, a challenge heightened when coupled with the introduction of implants. The tension dynamics in the peri-areolar region, a zone now tasked with harboring scars while maintaining a harmonious, symmetrical, and stable NAC, requires a meticulous, perhaps novel, approach to wound closure and tissue support.
Intriguingly, the potential solution may reside not within the conventional boundaries of aesthetic breast surgery, but in the realm of hand surgery. The Silfverskiöld technique, esteemed for its equitable tension distribution and enhanced repair stability in the milieu of tendon injuries, presents itself as a compelling candidate for adaptation and application within peri-areolar mastopexy. The essence of the Silfverskiöld repair, characterized by its ability to ensure even tension distribution and robust, stable closure in tendon repair, paves the path toward a hypothesis that its strategic implementation could mitigate areolar distortion and enhance the longevity and aesthetic quality of mastopexy-augmentation outcomes.
The principal aim of this study pivots around a meticulous examination of both immediate and long-term postoperative outcomes concerning NAC morphology, symmetry, and patient satisfaction, in cases where the Silfverskiöld technique has been adapted for NAC closure and support.
Methods
Study design
1. This retrospective case series analysed the outcomes of BA and PM employing the Silfverskiöld technique for NAC closure in patients with grade 1 ptosis operated upon between March and September 2022 at Enhance Medical Group, London, UK.
Surgical procedure
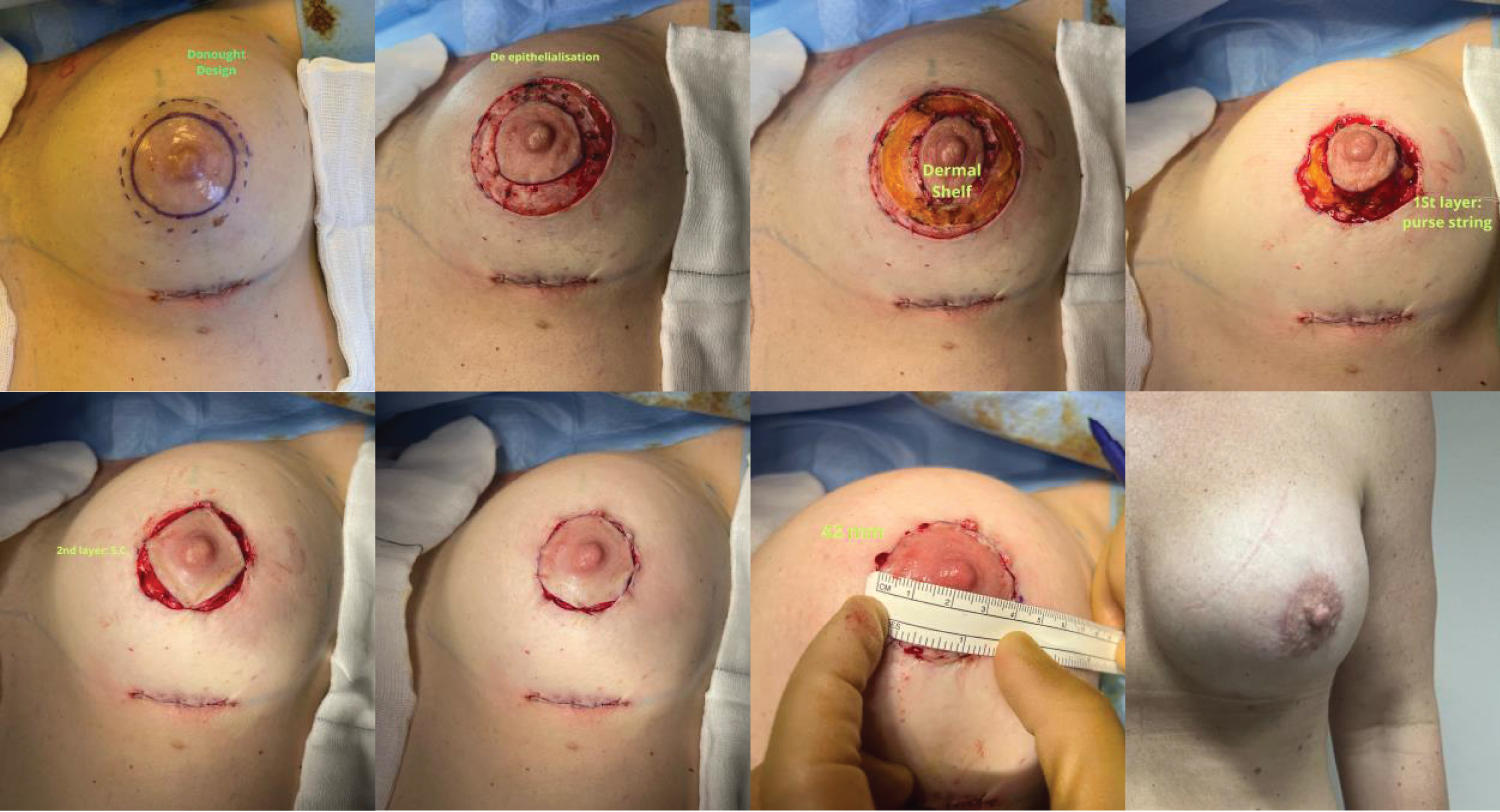
Each patient underwent a tailored peri-areolar mastopexy and breast augmentation performed by the senior author (MM). Implant specifications, pocket creation strategies, and a peri-areolar mastopexy using the Silfverskiöld technique for NAC closure were methodically documented for each patient. The surgical procedure initiated with breast augmentation, facilitated through an inframammary fold incision. The technique comprised a series of key steps (Figure 1), including the careful crafting of a doughnut-shaped incision around the NAC, precise de-epithelisation to aid the creation of a supportive dermal shelf, application of a purse-string suture using a continuous 3/0 monocryl on a reverse cutting needle, subcutaneous closure with interrupted 4/0 monocryl on a reverse cutting needle, and the meticulous use of the continuous locking Silfverskiöld with a 5/0 monocryl on a reverse cutting needle for NAC closure (Video 1).
Outcome measures
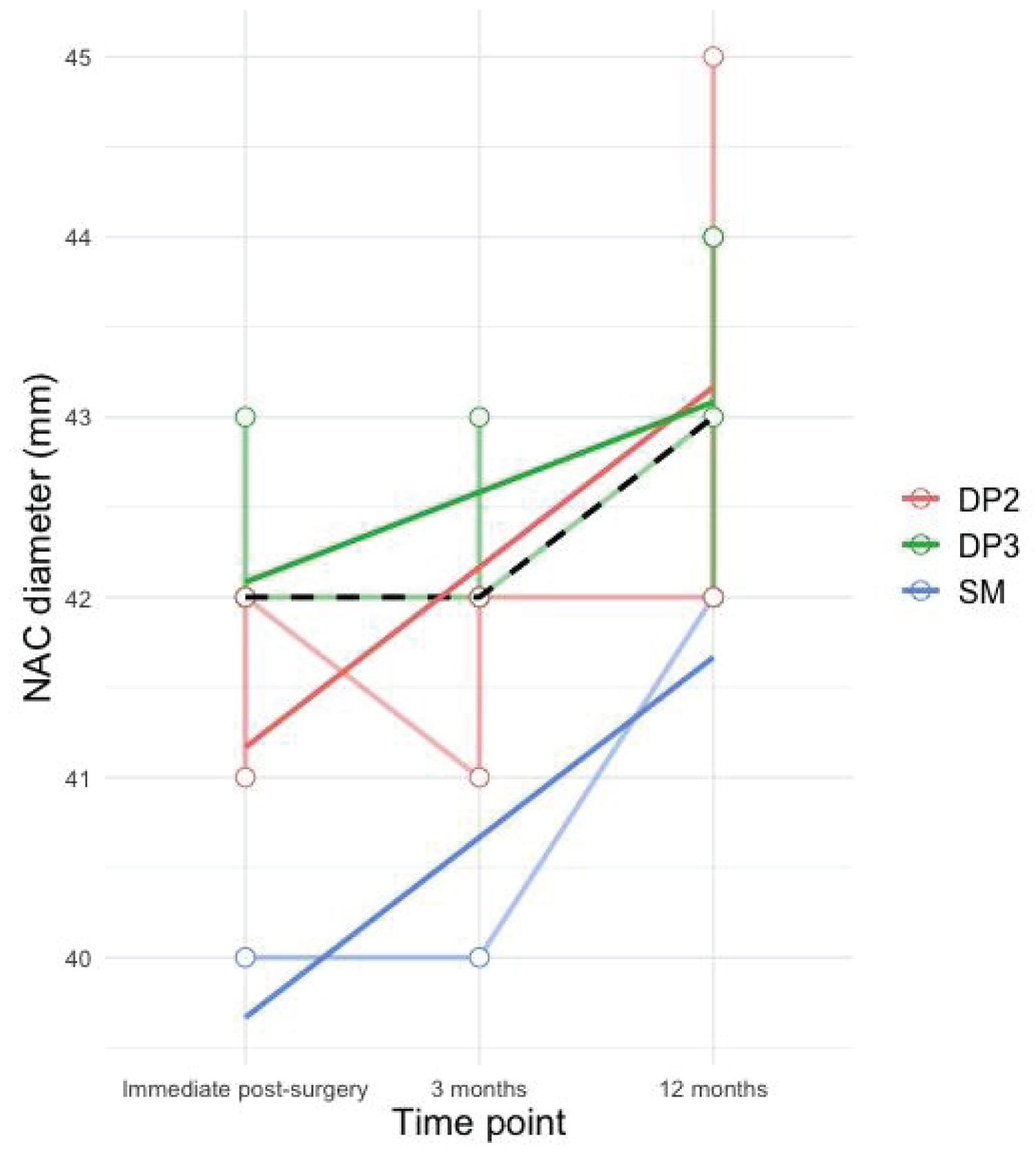
The primary outcome measures included NAC diameter (measured at the end of surgery, and at 3 months and 1-year post-operation), and general outcomes reflecting patient satisfaction and potential complications (Figure 2).
Statistical analysis
Longitudinal analysis will evaluate alterations in NAC diameters at various postoperative points, identifying trends and statistical significance across the time intervals. Concurrently, patient satisfaction will be quantitatively assessed through the calculation of categorical outcome frequencies, while a detailed investigation will seek to quantify and characterize any complications. The exploration of variations in the NAC diameter over time (immediately postoperatively, as well as 3- and 12-months post-operation) was undertaken to investigate changes over time. A linear mixed-effects model was implemented to facilitate this, providing a thorough exploration of shifts in NAC diameter at the predetermined intervals. Subsequently, an investigation into the influence of implant size and pocket technique on the NAC diameter at the 12-month postoperative point was conducted. Employing a linear regression model, relationships between the implant size, pocket technique, and NAC diameter were explored. This ensured a comprehensive understanding of the influence that both size and technique exerted on the final NAC diameter observed in patients. Statistical analysis was undertaken in R version 4.1.1 (R Core Team, R Foundation for Statistical Computing, Vienna, Austria). p < 0.05 was deemed statistically significant [1-3].
Results
Seven female participants, with a mean age of 39.4 years (range: 29-54), were enrolled in the study, each followed for a minimum of 12 months (Table 1). The mean implant size utilized was 359.29 cc (range: 240-545). Our surgical procedures encompassed a wide array of implant types and pocket techniques. These included the use of textured moderate plus implants with memory gel extra fill and textured high-profile implants. The pocket creation techniques employed encompassed dual plane procedures with varying depths (2/3) and submuscular approaches, exemplifying a tailored surgical approach for each individual case.
Immediately post-surgery, the median NAC (nipple-areolar complex) diameter measured 42.00 mm (40.00-43.00). Remarkably, at the 3-month follow-up, the median NAC diameter remained consistent at 42.00 mm (40.00-43.00). However, at the 12-month mark post-surgery, a slight increase in median NAC diameter was observed, reaching 43.00 mm (42.00-45.00). This change proved statistically significant when analyzed using a linear mixed effects model, revealing a noteworthy increase in NAC diameter from the immediate post-surgery period to both 3 months and 12 months post-surgery (3 months: estimate = -1.43, standard error = 0.31, degrees of freedom = 12.94, t-value = -4.55, p-value = 0.000553; immediate post-surgery: estimate = -1.43, standard error = 0.31, degrees of freedom = 12.94, t-value = -4.55, p-value = 0.000553).
Furthermore, our in-depth analysis sought to elucidate the potential impact of implant size and pocket technique on the final NAC diameter, as measured at the 12-month postoperative point. Employing a linear regression model, we found no statistically significant relationships between the ultimate NAC diameter and either implant size or pocket technique (implant size: p-value = 0.585; dual plane 3 pocket: p-value = 0.969; submuscular pocket: p-value = 0.570). The absence of statistical significance implies that, within the scope of this study, the selected implant size and pocket technique were not determinative factors influencing NAC diameter at the 12-month postoperative assessment.
Notably, there were no postoperative complications, and all patients expressed a high level of satisfaction, reporting a "very happy" sentiment upon discharge. This is exemplified with the before and after photos in Figure 3.
Discussion
In the realm of plastic and reconstructive surgery, the fusion of surgical techniques from diverse specialties often yields innovative advancements. This study delves into the innovation of applying the Silfverskiöld technique, primarily employed in hand surgery for tendon repair, to peri-areolar mastopexy-augmentation closure. Our aim was to address the enduring challenge of maintaining ideal NAC positioning and morphology, especially in the presence of implants.
The strength of our study lies in its meticulous examination of immediate and long-term postoperative outcomes. We assessed NAC morphology, symmetry, and patient satisfaction in cases where the Silfverskiöld technique was adapted for NAC closure and support. The results reveal a noteworthy increase in NAC diameter from immediate post-surgery to both 3 months and 12 months post-surgery. Although statistically significant, this increase is within a clinically acceptable range, suggesting the technique's effectiveness in minimizing NAC distortion. Moreover, our analysis explored the influence of implant size and pocket technique on the final NAC diameter at the 12-month postoperative point. The absence of statistically significant relationships implies that, within the scope of this study, neither implant size nor pocket technique served as determinative factors influencing NAC diameter. This suggests that the Silfverskiöld technique can provide stable NAC outcomes across a range of implant sizes and pocket techniques, making it a versatile option for surgeons. A notable strength of our study is the absence of postoperative complications and the high level of patient satisfaction, as all participants expressed a "very happy" sentiment upon discharge. This underscores the technique's safety and the favorable aesthetic results it can achieve.
Despite its strengths, this study has certain limitations. Firstly, it is a retrospective case series with a limited sample size, potentially affecting the generalizability of the findings. Further research with larger cohorts is warranted to confirm the technique's reproducibility and outcomes. Additionally, the study's follow-up duration was limited to 12 months, and longer-term outcomes should be investigated to assess the technique's durability. Comparative studies that evaluate the Silfverskiöld technique against other NAC closure methods in mastopexy-augmentation procedures could further validate its advantages.
Conclusion
The adaptation of the Silfverskiöld technique to peri-areolar mastopexy-augmentation closure shows promise in minimizing areolar distortion and maintaining stable NAC outcomes. With further research and refinement, this interdisciplinary approach has the potential to enhance the aesthetic quality and longevity of such procedures.
References
- Silfverskiöld KL, May EJ (1994) Flexor tendon repair in zone II with a new suture technique and an early mobilization program combining passive and active flexion. J Hand Surg Am 19: 53-60.
- Baran CN, Peker F, Ortak T, et al. (2001) Unsatisfactory results of periareolar mastopexy with or without augmentation and reduction mammoplasty: Enlarged areola with flattened nipple. Aesthet Plast Surg 25: 286-289.
- Benelli L (1990) A new periareolar mammaplasty: The ‘round block’ technique. Aesthet Plast Surg 14: 93-100.
Corresponding Author
Mohamed Maklad, Enhance Medical Group, London, UK.
Copyright
© 2024 Ali SR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.