Comparison of Long-Term Survival, Mortality, and Predictors of Mortality in Patients with One-Stage and Two-Stage Fontan Surgery: A Systematic Review
Abstract
Background: Techniques and strategies in the Fontan procedure have evolved over the years, including the evolution from a one-stage to a two-stage procedure. As such adjustments are made; attention must turn to survival analysis, including bidirectional cavopulmonary shunt (BCPS) and inter-stage mortality. However, whether this procedure should be performed as a one-stage procedure or a two-stage procedure is still a matter of debate despite many recent studies showing the benefits of a two-stage procedure, especially in high-risk cases.
Objectives: This study aims to compare the effect of better outcomes including long-term patient survival, mortality rate, length of ICU stay, and predictors of mortality between patients undergoing one-stage and two-stage Fontan surgery.
Methods: We included a retrospective analysis of Randomized Control Trials (RCTs) from the last 12 years (2011-2023) that assessed the comparison between the outcomes of one-stage and two-stage Fontan surgery. Several databases (PubMed, Wiley, and ScienceDirect) were thoroughly reviewed. This study was a systematic review that followed the PRISMA guidelines.
Discussion: 17 titles were included in this study. These studies compared the clinical superiority of the two-stage versus one-stage modified Fontan procedure in terms of long-term survival, mortality rate, ICU length of stay, and predictors of death. There was a better clinical advantage in pediatric patients over 2 years of age undergoing the 2-stage modified Fontan procedure in terms of lower mortality rate, improved oxygen saturation, decreased volume load, and less atrioventricular valve regurgitation as well as relatively shorter Length of Stay (LOS) compared to single-stage.
Conclusion: The analysis found that a two-stage modified Fontan procedure with Bidirectional Glenn shunt (BDG) intervention may provide a higher probability of success in palliative therapy in patients with single ventricle.
Keywords
Univentricular heart, Single ventricle, Fontan procedure, Cardiopulmonary bypass, Length of ICU stay, Mortality, Systematic review
Introduction
The Fontan operation was first described in 1971 and has become a standard procedure for a wide variety of complex congenital heart diseases, particularly hearts with single ventricle physiology as well as other complex cardiac malformations with 2 complete or incomplete ventricles when biventricular surgery is not possible. Several modifications have been introduced to reduce surgical mortality, decreasing length of stay, and prolonging patient survival. In 1988, de Leval [1] started to implement Total Cavopulmonary Connection (TCPC) or lateral tunnel which describes the connection of blood flow from the Inferior Vena Cava (IVC) directed to the Pulmonary Artery (PA) through an intra-atrial tunnel consisting of a prosthetic baffle joining the atrial walls. Marcelletti, et al. [2] in 1990 described a total cavopulmonary junction procedure using an extra-cardiac conduit from the IVC to the PA. The extra-cardiac conduit procedure provided superior hemodynamics compared to the intra-atrial lateral tunnel and extra-cardiac tunnel techniques. The hemodynamic advantage is greatly enhanced by the use of conduits to the superior vena cava; especially at physiologically high flows such as occur during exercise. With modification of the procedure, both lateral channels and extra-cardiac channels have been used in both groups. We review the surgical outcomes of the modified one-stage and two-stage Fontan procedures to clarify the clinical advantages.
Methods
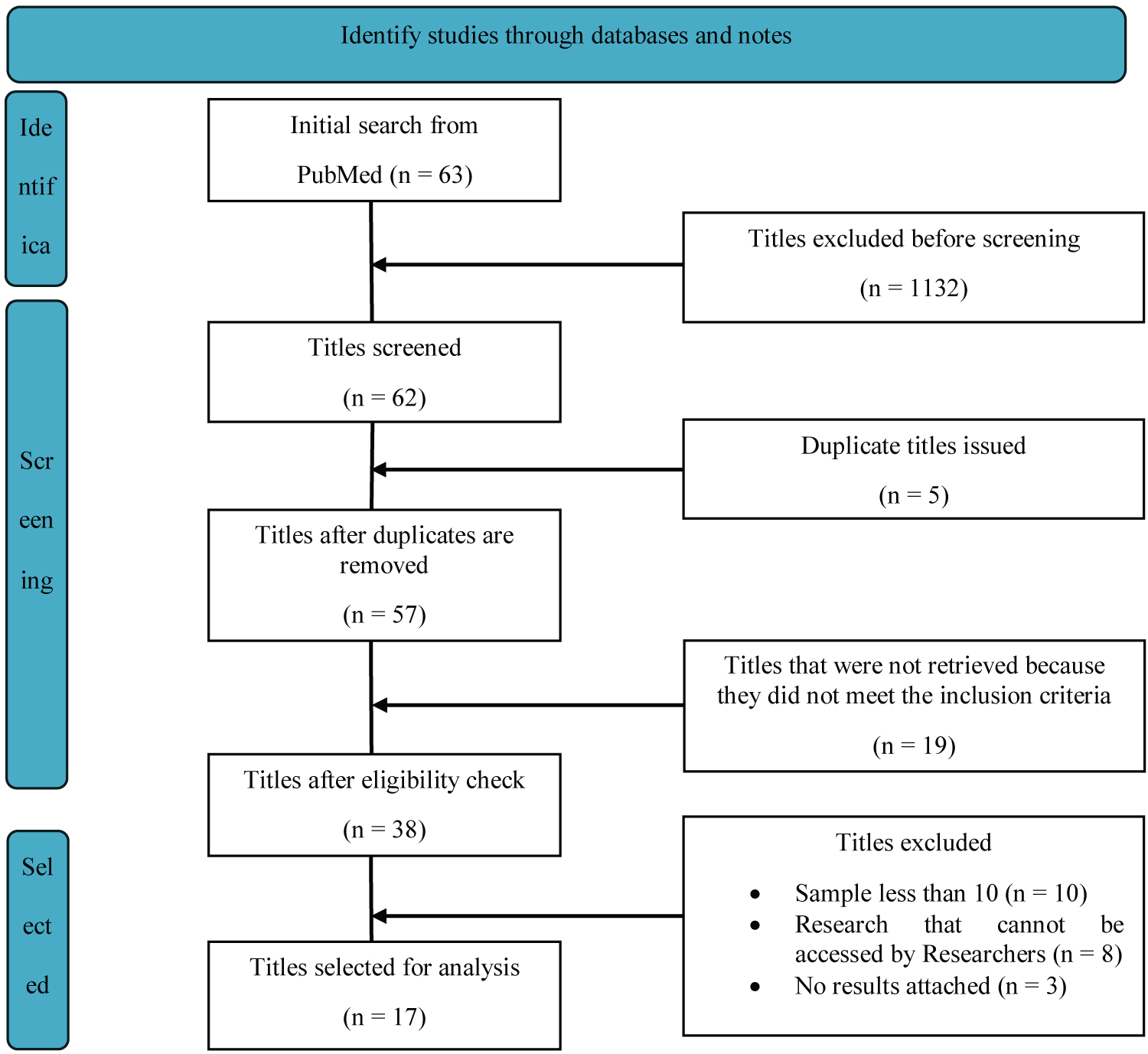
We conducted a comprehensive search, through electronic databases searched from PubMed, Wiley, and ScienceDirect then conducted an advanced search on each database. Data obtained from PubMed totaled 63 titles, Wiley obtained 679 titles, and ScienceDirect obtained 452 titles. The titles were then screened with 1132 titles then excluded from the study, then 62 titles were screened again and 5 duplicate titles were found which were then excluded, after being excluded there were 57 titles checked, and there were 19 titles that did not meet the inclusion criteria. The eligibility of 38 titles was checked and 21 titles were found that did not meet the inclusion criteria. The selected titles were then identified and descriptively analyzed from the final 17 titles that met the inclusion criteria in this study (Figure 1).
To facilitate journal searches, the PICO (Population, Intervention, Comparison, and Outcomes) search model was used to facilitate the development of searches to organize systematic reviews (Table 1).
Inclusion and exclusion criteria
The inclusion criteria of this study are:
1. Research with a retrospective design published in the last 12 years (May 2011 to January 2023) due to limited sources of information about the research conducted.
2. The included studies were following the journal search strategy.
3. Studies that used samples of children from 0 to 18-years-old.
4. English and Indonesian Language Research
The exclusion criteria of this study are:
1. Research with less than 10 samples.
2. Studies that cannot be accessed by researchers or are not full-text.
3. Studies with incomplete results.
Discussion
In the current era, definitive palliation therapy for complex cardiac anomalies with a functional single ventricle usually involves different modifications to the Fontan procedure and TCPC with an extra-cardiac conduit is an attractive option. One of the major advances in the last decade that resulted in a significant reduction in morbidity and mortality after the modified Fontan/TCPC procedure was the concept of TCPC staging with the previous bidirectional glenn procedure. Polat, et al. [3] in 2023 conducted a retrospective study between 1995 and 2022 with a mean follow-up of 12 years (3 months-27 years). Attanavanich, et al. [4] used 28 pediatric patients who underwent the modified fontan procedure from October 1995 to October 2005, 15 patients had undergone a one-stage procedure and 13 patients had undergone a two-stage procedure. Results obtained Operative mortality was 26.6% in the stage 1 group and 0% in the stage 2 group. Mendoza, et al. [5] in 2012 using a retrospective design with 32 patients, who underwent fontan surgery between March 2000 and December 2009, said the hospital mortality rate was very low at 3% post-Fontan surgery. After a mean follow-up period of 44 months (interquartile range, 32-79), survival was 90%. Preoperative mean pulmonary artery pressure (measured during catheterization) correlated with advanced mortality. Of the remaining variables analyzed, the Nakata index and McGoon, as well as the duration of cardiopulmonary bypass (CPB) showed a high correlation with postoperative outcome. Interventional catheterization before Fontan surgery was performed in 42% of patients. Wolff D, et al. [6] in 2014 using a retrospective design reviewed 203 patients undergoing the Fontan procedure to complete the cavopulmonary junction between 1975 and 2011 and during a mean follow-up of 12 years, survival was 69%. The overall mortality rate decreased significantly over the last few decades (P = 0 .017). A study conducted by Kido, et al. [7] in 2021 using a retrospective design by identifying 556 patients who underwent BCPS between January 1998 and December 2019 found that 18 patients died while in the ICU, and 35 people died after discharge from the ICU. Decreased ventricular function was significantly associated with death during ICU stay (P = 0.002). In patients discharged alive from the ICU, LOS in the ICU [Hazard Ratio (HR) 1.04, Confidence Interval (CI) 95% 1.02-1.06; P < 0.001] and predominantly right ventricular (HR 2.41, 95% CI 1.03-6.63; P = 0.04) were independent risk factors for mortality. Analysis of receiver operating characteristics identified a cut-off value for ICU length of stay of 19 days. Mean pulmonary artery pressure (HR 1.03, 95% CI 1.01-1.05; P = 0.04) was a significant risk factor for ICU length of stay. Prolonged LOS in ICU with a cut-off value of 19 days after BCPS was a significant risk factor for mortality. High pulmonary artery pressure at BCPS was a significant risk factor for ICU length of stay.
A study conducted by Tamagond, et al. [8] in 2011 used a retrospective design in the period January 2001 to December 2009 with 15 patients (9 males and 6 females) undergoing single-stage TPCP. 31 patients underwent a direct BDG procedure of which 24 patients (14 males and 10 females) underwent TCPC completion 6 months to 26 months later. Staging of TPCP decreases postoperative mortality as evidenced by the studies conducted. Overall mortality in two-stage TCPC was lower than single-stage TCPC (4.2% in two-stage TP vs. 13.3% in single-stage TCPC). There was no mortality with early BDG in two-stage TCPC. TCPC had to be downgraded in 2 patients in one-stage TCPC. In two-stage TCPC completion, TCPC could not be performed in 5 patients due to high pulmonary artery pressure and low pulmonary artery pressure. Other postoperative outcomes were comparable in both groups.
The study of Chen H, et al. [9] in 2012 obtained midterm results (first 30 days after surgery and after surgery) on the Fontan procedure with direct cavopulmonary connection (DCPC) in several patients with functional univentricular heart using an Autologous pericardium patch on the atrial wall to facilitate one-stage and two-stage fontan extra-cardiac, especially with patients with the good pulmonary artery. 30 patients undergoing this type of surgery were retrospectively reviewed. There were 18 (60%) males and 12 (40%) females, with a mean age of 69 months (range 16-150 months) and a mean body weight of 23 kg (range 11-46 kg).
Aortic cross-clamping was used in 10 patients, with a median cross-clamp time of 40 minutes (range 23-99) and a median CPB time of 135 minutes (range 76-179 minutes). The remaining 20 patients were operated on without aortic cross-clamping. Their median CPB time was 104 minutes (range 78-139 minutes). Fenestration was performed on 16 patients. The follow-up period ranged from 2 months to 6 years. The rates of operative mortality and death after hospital discharge were zero. Major postoperative complications included supra ventricular tachycardia (SVT) in one patient, oliguria and peritoneal dialysis in one patient, and chest drainage (> 30 ml/day) lasting > 7 days in five patients (20%). One patient had sinus bradycardia due to a 2-month gap after hospital discharge. One patient developed pericardial effusion 1 month after discharge. The results showed a low risk of mortality and a low rate of re-intervention, but there were limitations to the study as no long-term intervention resulted in long-term patient survival. Zou, et al. [10] in 2015 reviewed data on patients who underwent TCPC procedures from January 2008 to December 2013. The estimated survival rate using the Kaplan-Meier analysis method over five years in the two-stage TCPC was significantly higher than the one-stage group (96.7% vs. 79.7%, P = 0.023). Mean Pulmonary Artery Pressure (mPAP) > 15 mmHg was associated with prolonged pleural effusion (> 14 days) and was a major determinant of postoperative hospital length of stay. A study conducted by Ovroutski, et al. [11] and colleagues also showed that a Nakata index below 150 mm 2 /m 2 correlated with unfavourable outcomes. Hosein, et al. [12] reviewed the outcomes of 406 patients over 16 years and found that the two significant risk factors for fontan procedures from baseline and end line were impaired ventricular function preoperatively and mPAP > 15 mmHg. Many studies have revealed that staged procedures can reduce morbidity and mortality, especially for patients who will undergo fontan in the high-risk category [13].
Conclusion
Older pediatric patients (> 2 years) undergoing a 2-stage modified Fontan procedure have better outcomes in terms of lower mortality, improved oxygen saturation, decreased cardiac volume load, and less atrioventricular valve regurgitation and relatively short LOS compared to single-stage fontan.
Funding
This work received no specific grants from any funding agency in the public, commercial, or non-for-profit sectors.
Declaration of Conflicting Interest
None declared.
References
- de Leval MR, Kilner P, Gewillig M, et al. (1988) Total cavopulmonary connection: A logical alternative to atriopulmonary connection for complex fontan operations. Experimental studies and early clinical experience. J Thorac Cardiovasc Surg 96: 682-695.
- Marcelletti C, Corno A, Giannico S, et al. (1990) Inferior vena cava-pulmonary artery extracardiac conduit. A new form of right heart bypass. J Thorac Cardiovasc Surg 100: 228-232.
- Polat A B, Erturk M, Uzunhan O, et al. (2023) 27 years of experience with the fontan procedure: Characteristics and clinical outcomes of children in a tertiary referral hospital. J Cardiothorac Surg 18: 38.
- Attavanich S, Limsuwan A, Vanichkul S, et al. (2007) Single-stage versus two-stage modified fontan procedure. Asian Cardiovasc Thorac Ann 15: 327-331.
- Alberto M, Leticia A, Enrique R, et al. (2012) Fontan operation. Hemodynamic factors associated with postoperative outcomes. Rev Esp Cardiol (Engl Ed) 65: 356-362.
- Wolff D, van Melle JP, Ebels T, et al. (2014) Trends in mortality (1975-2011) after one- and two-stage fontan surgery, including bidirectional glenn through fontan completion. Eur J Cardiothorac Surg 45: 602-609.
- Kido T, Ono M, Anderl L, et al. (2021) Factors influencing length of intensive care unit stay following a bidirectional cavopulmonary shunt. Interact Cardiovasc Thorac Surg 33: 124-130.
- Tamagond S, Agarwal S, Prakash S, et al. (2021) Single stage versus two stage repair for univentricular heart-our experience. Indian J Thorac Cardiovasc Surg. (April-June 2011) 27: 83-87.
- Chen H, Hong H, Zhu Z, et al. (2013) Extracardiac fontan with direct cavopulmonary connections: Midterm results. Eur J Cardiothorac Surg 43: 318-323.
- Zou M, Wang Y, Cui H, et al. (2016) Outcomes of total cavopulmonary connection for single ventricle palliation. J Thorac Dis 8: 43-51.
- Ovroutski S, Ewert P, Alexi-Meskishvili V, et al. (2009) Absence of pulmonary artery growth after fontan operation and its possible impact on late outcome. Ann Thorac Surg 87: 826-831.
- Hosein RB, Clarke AJ, McGuirk SP, et al. (2007) Factors influencing early and late outcome following the fontan procedure in the current era. The 'Two Commandments'? Eur J Cardiothorac Surg 31: 344-352.
- Bridges ND, Jonas RA, Mayer JE, et al. (1990) Bidirectional cavopulmonary anastomosis as interim palliation for high-risk Fontan candidates. Early results. Circulation 82: IV170-176.
Corresponding Author
Suprayitno Wardoyo, Division of Cardiothoracic Surgery, Department of Surgery, University of Indonesia, Jakarta, Indonesia, Tel: 081213158732.
Copyright
© 2024 Wardoyo S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.