Surgical Management of Unruptured Sinus of Valsalva Aneurysm Detected Incidentally after Repair of Tetralogy of Fallot - A Case Report
Abstract
Sinus of Valsalva Aneurysms (SOVA) represents dilation of one or more of the three aortic sinuses. The occurrence of SOVA after repair of Tetralogy of Fallot (TOF) is rare. It can be detected during routine follow up. Detailed imaging is necessary to plan surgical procedure. Unruptured aneurysm should be repaired by appropriate surgical technique depending on its anatomy. Concomitant pulmonary valve replacement is necessary when indicated. We present a case of a 20-year-old man who was operated for repair of TOF in infancy. He was incidentally detected to develop unruptured SOVA of right aortic sinus during routine follow up echocardiography and underwent successful surgical repair.
Keywords
Sinus of valsalva aneurysm, Tetralogy of fallot, Unruptured, Right aortic sinus, Pulmonary valve replacement
List of Abbreviations
SOVA: Sinus of Valsalva Aneurysm; TOF: Tetralogy of Fallot; RVOT: Right Ventricular Outflow Tract; CPB: Cardiopulmonary Bypass; LVOT: Left Ventricular Outflow Tract
Introduction
Sinus of Valsalva Aneurysm (SOVA) is defined as dilation of one or more of the three aortic sinuses which form the connection between aortic valve and ascending aorta [1]. The association of SOVA with Tetralogy of Fallot (TOF) is uncommon [2,3] and occurrence of SOVA after repair of TOF is rare [4,5]. We report a successful repair of unruptured SOVA in a 20-year-old patient who was operated for repair of TOF in infancy.
Case Presentation
A twenty-year-old man was operated for repair of TOF with Trans-annular patch at the age of 9 months. He was a known case of DiGeorge syndrome. He was under regular follow up with echocardiography at 6 months interval for evaluation of progressive pulmonary regurgitation and dilatation of right ventricle. He was otherwise asymptomatic. His recent echocardiography demonstrated an aneurysmal out pouching of right sinus of valsalva into right ventricular outflow tract (RVOT). There was severe pulmonary regurgitation with moderately dilated right ventricle with preserved biventricular systolic function.
CT scan (Figure 1) showed that the aneurysm was arising from left side of the base of right coronary sinus which was indenting the RVOT. The neck measured 16 mm and the sac measured 10 mm. There was no defect or any evidence of shunting. The origin of Right Coronary Artery was 8.5 mm above the superior wall of the aneurysm. Based on the imaging studies, the patient was planned for pulmonary valve replacement with re-inforcement of sinus of valalva aneurysm.
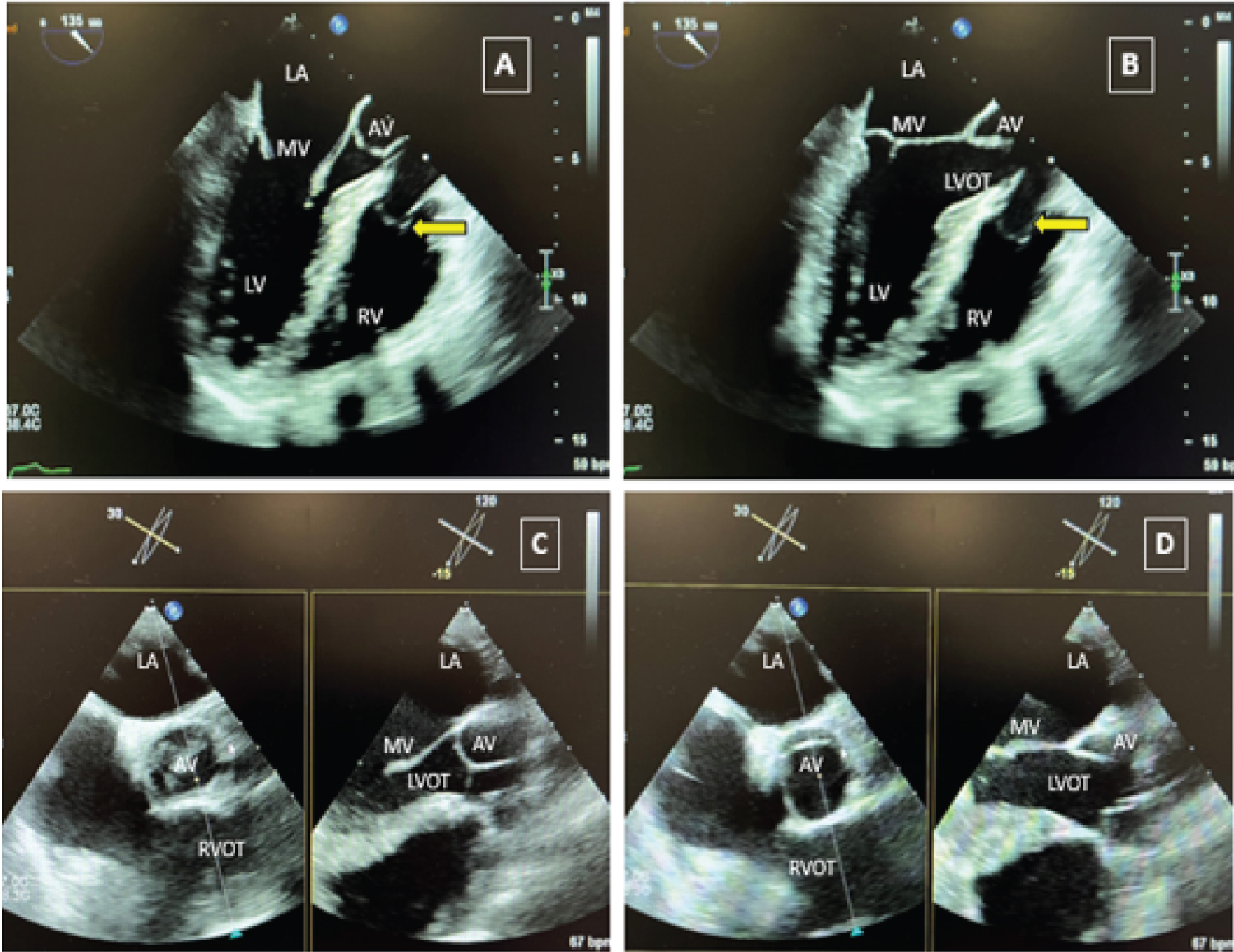
The sternal reentry was uneventful. Cardiopulmonary Bypass (CPB) was initiated with aorta and bicaval cannulation. The PA was opened with a longitudinal incision and anatomy was assessed. Only a remnant of posterior leaflet of pulmonary valve was detected. There was a large Sinus of Valsalva Aneurysm protruding into the RVOT at the level of below the pulmonary valve annulus (Figure 2). The edges of the aneurysm were identified. Following this the cross-clamp was applied and the cardioplegia was delivered. The aneurysm was repaired by plication of the windsock from the RVOT and reinforced by over sewing with pledgetted 4-0 polypropelene sutures. A 23 mm bio prosthetic valve was implanted at pulmonary position using a combination of continuous and interrupted polypropelene suture. The anterior part of the prosthesis was attached to the neo-annulus created from bovine pericardial patch used to repair the pulmonary artery. Heart regained activity in sinus rhythm after release of cross-clamp. Cardiopulmonary bypass was weaned off without any difficulty. On Transesophageal echocardiography after CPB, the valve was well seated in pulmonary position. The plication of aneurysmal sac was satisfactory without any flow across the sinus or any aortic incompetence (Figure 3). The RVOT was well opened. The patient was extubated shortly after surgery. He was discharged home following an uneventful recovery.
Discussion
The incidence of SOVA among mass is 0.09% and only 2% of the TOF patients are associated with SOVA [6,7]. In most of the cases it is diagnosed incidentally [6]. In our patient it was detected during routine follow up echocardiography. When symptomatic, they are often associated with rupture of the aneurysm which result in significant morbidity and mortality due to complications like arrhythmias, ischemia and thromboembolic events [8]. Right Coronary Sinus is most commonly involved in the aneurysm formation and requires early surgical intervention due to higher incidence of rupture [6].
Transthoracic echocardiography is considered as the initial investigation of choice [8]. Following repair of TOF it is important to assess the anatomy of SOVA with its potential effect on RVOT obstruction and Left Ventricular Outflow Tract (LVOT) distortion, function of aortic and pulmonary valve and right ventricular function and volumes due to free pulmonary regurgitation. A wide pulse pressure across the RVOT due to progressive free pulmonary regurgitation may have a negative suction effect on the right coronary sinus resulting in formation of the SOVA. A preoperative CT scan can be obtained to delineate the anatomy of the aneurysm in detail and its relation with surrounding structures including origin of coronary arteries and also to plan surgical repair technique. Trans-esophageal echocardiography has also been a recommended subsequent investigation [8]. Mid-esophageal Aortic valve long axis view is helpful intraoperatively in demonstrating aortic valve function, adequacy of leaflet coaptation, any stenosis or regurgitation of aortic valve before and after surgical repair of aneurysm [9]. Various types of repair techniques have been described in literature. When anatomy is favourable, unruptured aneurysm can be plicated with or without reinforcing sutures [1]. Pericardial patch repair technique has been mentioned by Takach, et al. [10]. Aortic valve may need some form of repair or replacement depending on its pre-operative condition and distortion due to proximity to the aneurysm repair site [10]. When Aortic valve repair is required, coaptation length of more than 4 mm is associated with better prognosis and less chance of aortic regurgitation in future [9]. In our case the aneurysm was repaired by plication from the RVOT side followed by reinforcement suture along with bio prosthetic pulmonary valve replacement for free pulmonary regurgitation. The post-repair Trans-esophageal echocardiography was satisfactory.
To summarise, occurrence of SOVA after repair of TOF is unusual and can be detected during routine follow up. Detailed imaging is necessary to plan surgical procedure. Unruptured aneurysm should be repaired by appropriate surgical technique depending on its anatomy. Concomitant Pulmonary valve replacement is necessary when indicated.
Acknowledgements
We acknowledge help from our colleagues from department of Cardiac Imaging and Cardiology (Adult Congenital Heart Disease).
Financial Support
This work received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
The author(s) declare no conflicts of interest.
References
- Nguyen Q, Vervoort D, Phan K, et al. (2021) Surgical management for unruptured sinus of valsalva aneurysms: A narrative review of the literature. J Thorac Dis 13: 1833-1850.
- Talwar S, Chigurupati BS, Choudhary SK (2018) Ruptured sinus of valsalva aneurysm with tetralogy of fallot in an adult. J Card Surg 33: 688-690.
- Mithani AA, Polimenakos AC, Santucci BA (2013) Ruptured sinus of valsalva found incidentally in a patient with tetralogy of fallot. Pediatr Cardiol 34: 1914-1917.
- Talwar S, George N, Kothari SS, et al. (2020) Ruptured sinus of valsalva presenting late following repair of tetralogy of fallot. J Card Surg 35: 1690-1693.
- Balducci A, Gesuete V, Fabi M, et al. (2011) An unusual case of sinus of valsalva aneurysm in a guch patient: An unusual side of the aorto-cardiac fistula. Cardiol Res 2: 193-195.
- Weinreich M, Yu PJ, Trost B (2015) Sinus of valsalva aneurysms: Review of the literature and an update on management. Clin Cardiol 38: 185-189.
- Vural KM, Sener E, Tasdemir O, et al. (2001) Approach to sinus of valsalva aneurysms: A review of 53 cases. Eur J Cardiothorac Surg 20: 71-76.
- Feldman DN, Roman MJ (2006) Aneurysms of the sinuses of valsalva. Cardiology 106: 73-81.
- Hall T, Shah P, Wahi S (2014) The role of transesophageal echocardiography in aortic valve preserving procedures. Indian Heart J 66: 327-333.
- Takach TJ, Reul GJ, Duncan JM, et al. (1999) Sinus of valsalva aneurysm or fistula: Management and outcome. Ann Thorac Surg 68: 1573-1577.
Corresponding Author
Sayar Kumar Munshi, MBBS, MS, MCH, Department of Paediatric Cardiac Surgery, Alder Hey Children's Hospital, Liverpool, Apartment 4, Generation House, Station Road, 32 Station Road, South Gosforth, Newcastle Upon Tyne, NE3 1QD, UK, Tel: +44-7887323553.
Copyright
© 2024 Munshi SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.