VATS Trisegmentectomy Resection of Aspergilloma with Pan-Azole Resistance?
Abstract
Pulmonary aspergillosis is a relatively rare disease and its management is sometimes difficult. Surgical resection is indicated in selected patients. We present a nationally unreported case (to the best of our knowledge) of VATS anatomical sublobar lung resection for isolated left upper lobe aspergilloma in a 55-year-old male with history of chronic pulmonary aspergillosis (CPNA). As adhesions prove to be a significant intra-operative obstacle, VATS segmentectomy can be ambitious, however this can be considered for simple aspergilloma in absence of severe pleural adhesions.
Keywords
Aspergillus, VATS, Trisegmentectomy, Aspergillosis
Background
Aspergillomas (fungus balls) are inflammatory lung processes, and as such are often associated with intrathoracic adhesions [1]. Pleuro-parenchymal adhesions increase significantly the technical difficulty of segmental resections in aspergillomas. These have classically been approached via thoracotomy due to the impact on operative time and potential risks of a substantial air leak and haemorrhage. Recently, video-assisted thoracoscopic surgery (VATS) approaches have been successfully adopted for lobectomy and segmentectomy overseas [2]. We describe the first UK case of a VATS left upper lobe trisegmentectomy for isolated aspergilloma.
Case Report
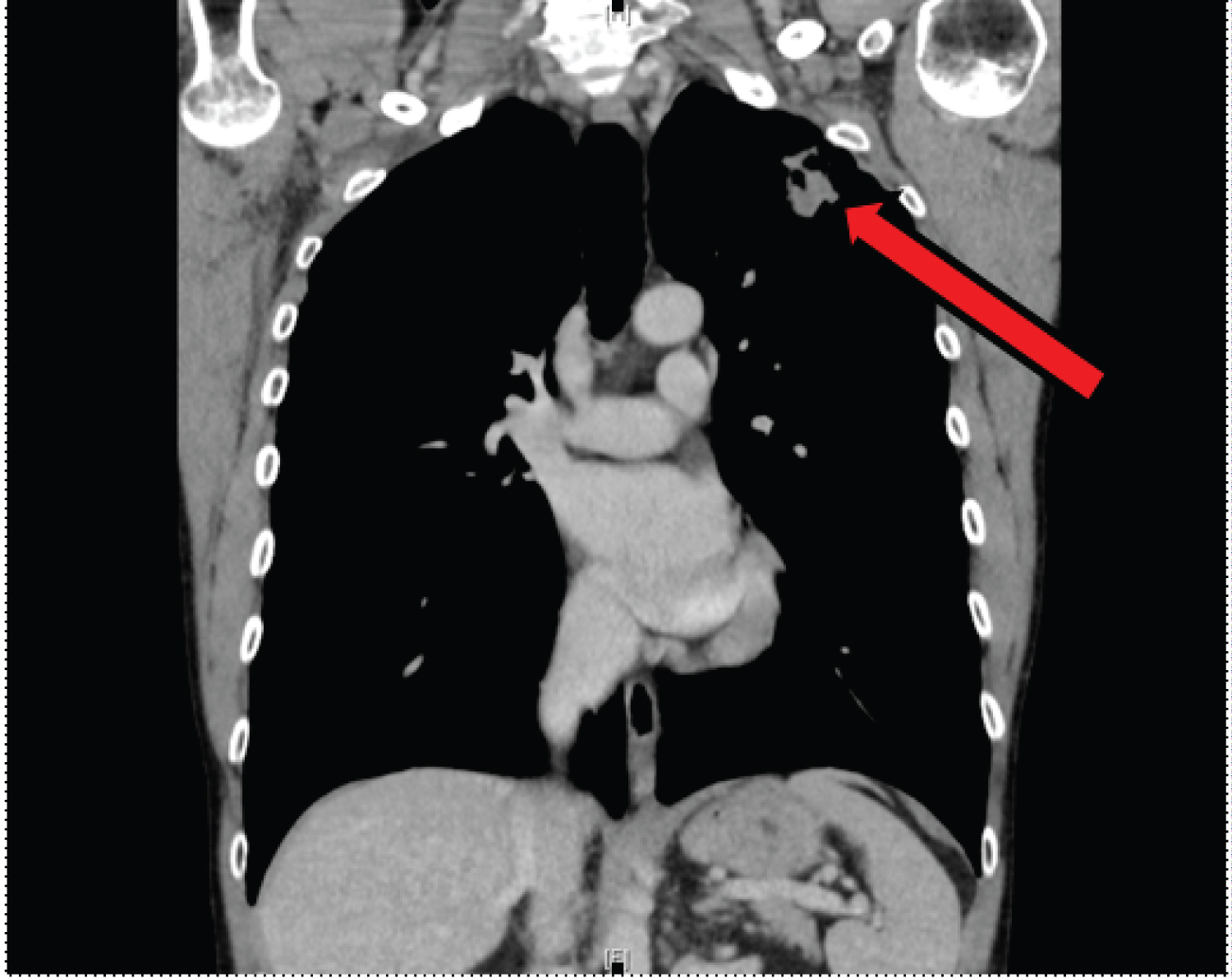
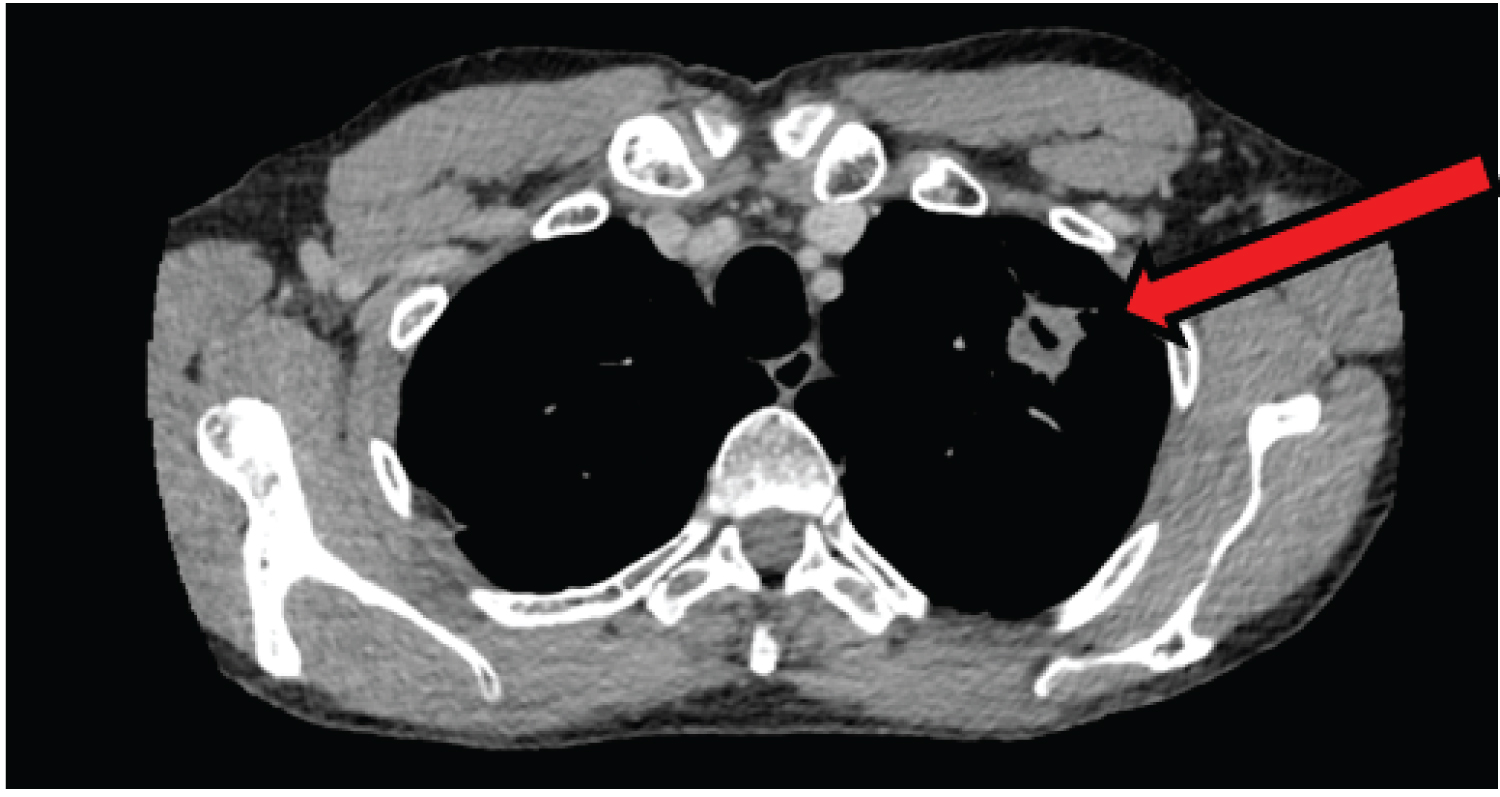
We report the case of a 55-year-old male under the care of the National Aspergillosis Centre with an established diagnosis of a simple pulmonary aspergilloma that was being monitored and controlled with oral itraconazole. The latest chest CT scan showed a simple left upper lobe aspergilloma (Figure 1), which had become thinner compared to previous scans. Therefore, surgical resection appeared amenable resection. This was confirmed after discussion in the lung multidisciplinary team.
His past medical history included lifelong asthma (for which he took a regular beclometasone/formeterol inhaler), allergic bronchopulmonary aspergillosis and hypertension (possibly aggravated by itraconazole). Patient's performance status was 0 and he was managing an active lifestyle regularly playing badminton and tennis.
Due to the growth of pan-zole resistant Aspergillus fumigatus itraconazole was stopped and he was assessed for surgical resection after intravenous antifungal treatment.
Given the peripheral location of the aspergilloma, it was decided that a minimally invasive approach would be attempted and a parenchymal sparing anatomical left upper lobe trisegmental resection would be attempted. A 3-port VATS technique was used with a single port inserted primarily to evaluate whether VATS would be feasible. As only minor apical adhesions were found, we proceeded with VATS and completed the entire operation without any complications. The postoperative course was uneventful, and in-hospital discharge was at 5th day after operation. The histopathological findings confirmed the diagnosis of completely resected aspergilloma. He made an excellent recovery and returned to his baseline level of function. Seven months following the left upper lobe trisegmentectomy, he was fully active and back to his baseline of activities. Serum aspergillus IgG antibodies (ImmunoCap) had also fallen from a high of 121 mg/l to 37 mg/l (normal < 40 mg/L) indicating complete resection and cure.
Discussion
Simple aspergilloma is one sub-type of chronic pulmonary aspergillosis. Symptoms may be improved with oral azole antifungal therapy, however surgical resection is the only true and complete cure for the patients [3]. Development of azole resistance, as in this case, is all too often especially with a large fungal load as in patients with aspergillomas. Lobectomy is the commonest procedure, but results in loss of surrounding normal lung. By adopting a VATS trisegmentectomy approach, more lung is preserved and the risk of post-surgical pain over the operative site is reduced. In this case, the post-operative recovery after removal of a simple pulmonary aspergilloma was rapid, without any complications.
Generally, the main issue with performing VATS in aspergilloma is the presence of severe intrathoracic pleuro-parenchymal adhesions preventing adequate space for safe lung resection, which is further compounded when attempting segmentectomy to spare lung function; particularly of the upper lobes [4]. Despite these limitations, lobectomies [5], wedge resections and segmentectomies [6] have been carried out using VATS in other countries. Segmentectomy should be preferred when the aspergilloma is simple and at the periphery of the lung parenchyma to allow for preservation of lung function [7] as seen in our case (Figure 1 and Figure 2). The current practice guidelines of European Society for Clinical Microbiology and Infectious Diseases and European Respiratory Society recommend surgical resection for selected cases of simple aspergilloma [8].
In conclusion, we believe this is the first case of sublobar anatomical lung resection performed in the United Kingdom for aspergilloma. We argue that anatomical lung resection can be carried out safely via VATS after initial assessment of intra-operative adhesions. Larger database is necessary to formulate more specific recommendations.
Funding
We received no funding.
Conflict of Interest
There is no conflict of interest.
References
- Moodley L, Pillay J, Dheda K (2014) Aspergilloma and the surgeon. J Thorac Dis 6: 202-209.
- Chen QK, Jiang GN, Ding JA (2012) Surgical treatment for pulmonary aspergilloma: A 35-year experience in the Chinese population. Interact Cardiovasc Thorac Surg 15: 77-80.
- Farid S, Mohammed S, Devbhandari M, et al. (2013) Surgery for chronic pulmonary aspergillosis, risk stratification and recurrence - A National Centre's experience. J Cardiothorac Surg 8: 180.
- Chen QK, Chen C, Chen XF, et al. (2014) Video-assisted thoracic surgery for pulmonary aspergilloma: a safe and effective procedure. The Annals of Thoracic Surgery 97: 218-223.
- Parker KL, Zervos MD, Darvishian F, et al. (2010) Video-Assisted Thoracoscopic Lobectomy for Pulmonary Aspergilloma After Life-Threatening Hemoptysis in a Patient With Lupus. The Annals of Thoracic Surgery 89: 291-292.
- Whitson BA, Maddaus MA, Andrade RS (2007) Thoracoscopic lingulectomy for invasive pulmonary aspergillosis. Am Surg 73: 279-280.
- Soukiasian HJ, McKenna RJ (2014) Minimally invasive VATS left upper lobe apical trisegmentectomy. Ann Cardiothorac Surg 3: 194-196.
- Denning DW, Cadranel J, Beigelman-Aubry C, et al. (2016) Chronic pulmonary aspergillosis-rationale and clinical guidelines for diagnosis and management. Eur Resp J 47: 45-68.
Corresponding Author
Muhammad Asghar Nawaz, Department of Cardiothoracic Surgery, Wythenshawe Hospital NHS, Manchester Foundation Trust, Manchester M23 9LT, UK
Copyright
© 2021 Nawaz MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.