The "Slim-Mesh": Single Operation with Multiple Slim-Meshes for Multiple Widely-Spaced Ventral Hernias in the Same Patient
Abstract
Purpose: Test the technical feasibility of the "Slim-Mesh" technique using multiple "Slim-Meshes" during an operation for multiple widely-spaced ventral hernias in the same patient; verify the results of a 12-year followup.
Methods: From September 2009 to December 2019, 8 patients with the above hernias were treated exclusively with the "Slim-Mesh" technique at our Department. This was a prospective (63%)-retrospective study.
Results: This study comprised 6 males and 2 females. Mean age was 57 years. Three of the 8 cases had a triple spaced ventral hernia (Group 1): 2 of the 3 were treated with 2 "Slim-Meshes" each, and the remaining patient with 3. The remaining 5 cases had one double spaced ventral hernia each (Group 2); each case was operated on with 2 "Slim-Meshes". During operation, the author also found and repaired associated diastasis recti in 38% of cases, doing so without using additional "Slim-Meshes". Mean operation time for all 8 cases, Group 1 and Group 2 was 153, 220 and 112 minutes respectively. Composite mesh, non-composite mesh, titanium tacks and absorbable straps for mesh fixations were used in 87.5%, 12.5%, 25% and 75% of cases respectively. Mean length of hospital stay was 3 days. Mean follow-up time was 6 years. No early or long-term postoperative complications occurred.
Conclusion: This study revealed the existence of a new patient-type, namely one with multiple widely-spaced ventral hernias (7%). My technique facilitates intra-abdominal introduction and fixation of successive multiple meshes during the same operation, proving to be safe, fast and economical.
Keywords
Multiple widely-spaced ventral hernia, Slim-mesh technique, Multiple slim-meshes, Operation time, Ergonomic multiple widely-spaced ventral hernia repair
Introduction
The abdominal-wall (AW) is sometimes mistakenly considered as the entrance-door to a patient's abdomen when surgeons perform laparotomy to access and operate on the intra-abdominal organ related to their specialization. On the contrary, the AW is a large and complex body-part consisting of multiple organs, such as skin, subcutaneous adipose tissue, muscle fasciae, muscles, vessels/nerves and linea alba and contributes to the performance of all our daily activity [1]. Laparotomy is performed by many types of surgeons [2], including liver and kidney transplant surgeons, urologists, gynecologists [2], vascular-, esophageal-, colorectal-, liver-, pancreatic-, cancer-, AW-, bariatric-, thoracic- and neuro-surgeons. They may carry out several different types of laparotomy, which can be median laparotomy with xiphoid-pubic incision, the Mercedes Benz-type incision [3], mini-median-type, sub-costal unilateral [4,5]/bilateral sub-costal laparotomy [6], the pararectus abdominis approach [7], the Pfannenstiel incision [8], mini-mini laparotomy for peritoneal drainage placement in thoracic/abdominal open surgery, and mini-incision for trocar placement during laparoscopy (LAP, [9]). The surgical closure of these laparotomies can be quite different [2] and tends to lead to an incisional hernia in just over half of cases [10-12]. In case of multiple laparotomies in the same patient, more than one incisional hernia may develop at the laparotomy sites [3], appearing as widely-spaced. Sometimes a spaced primary ventral hernia (VH), e.g. an umbilical hernia, and/or diastasis recti abdominis (DR) [13], may develop, too. We named this type of AW defect a "multiple widely-spaced ventral hernia" (MWSH).The MWSH patient can experience the typical symptoms of a VH in different parts of the AW, such as pain and bulging, in association with vomiting, constipation, intestinal obstruction and strangulation [14].
The front muscles of the AW generates forces acting simultaneously and in balance with the rear muscles of a human being's trunk so that he/she can perform normal vital functions of everyday life, such as working, standing, walking, running, lifting weights [15]. Furthermore, MWSH can cause a great loss of AW function, with associated imbalance of the forces generated by the front/rear muscles of the trunk and the diaphragm [15]. This AW dysfunction may lead to restricted everyday physical activity, respiratory and digestive disorders, abdominal-wall pain, back pain [16] due to spinal trouble, as well as urinary and obvious possible mood disorders. Consequently, MWSH could be considered a systemic disease.Firstly and empirically, the author wanted to test the technical feasibility and reliability of the "Slim-Mesh" (SM) technique with successive multiple SMs during an operation for the repair of MWSH located in the same patient, exploiting the well-known benefits of LAP combined with the SM technique's technical qualities [17-25]. Secondly, he expected to verify its outcomes in the MWSH patients with a 12-year follow-up study.
Materials and Methods
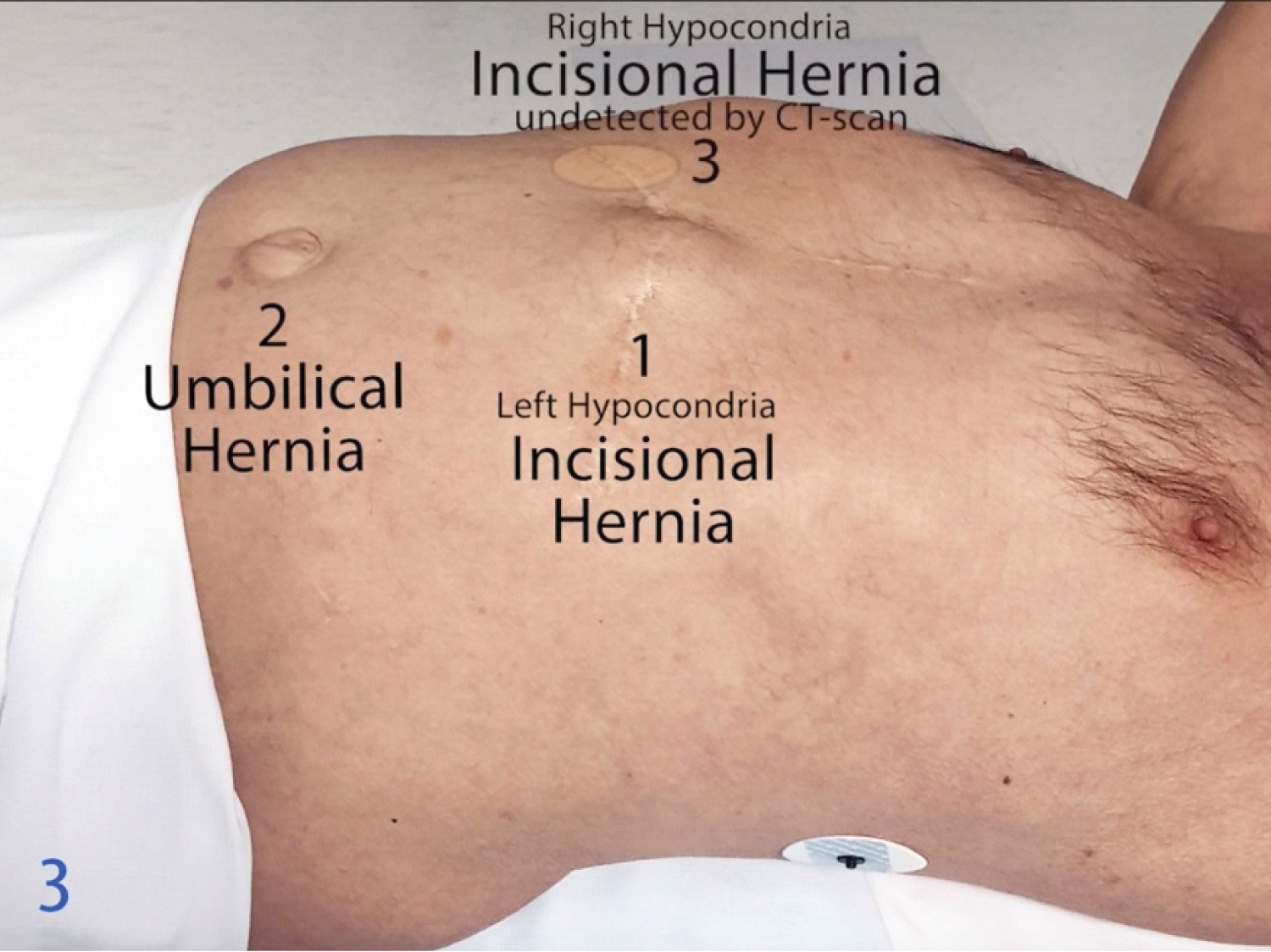
From September 2009 to December 2019, 8 patients with widely-spaced ventral hernia (MWSH) were treated by the author S.A.C. exclusively with the "Slim-Mesh" (SM) technique at his Department where different types of surgical diseases are treated. The 8 MWSH patients were selected to join the SM-protocol group of patients. The mesh used is called a ‘Slim Mesh' because of its thickness, becoming "slim cigarette like" [17-25], and not because of its composition or weight. The SM technique is divided into 4 surgical phases: phase 1 or first laparoscopic step, phase2: Marking the skin axial points (SAP), and the skin measurement of the SM application area (SMAA), which is the same as the peritoneal SMAA; phase 3: Preparation SM as per the SM technique, for introduction into the abdomen; phase 4 or last laparoscopic step [17-25]. S.A.C used successive multiple SMs (MSM) during an operation for the repair of MWSH located in the same patient. During the operation, he also found and repaired associated diastalsis recti abdominis (DR), doing so without using additional SMS. He conducted this study in compliance with the principles of the Declaration of Helsinki. This was a prospective (63%) - retrospective study approved by Padua's Ethics Committee (contract no. 3902/AO/16) and a written informed consent was obtained from the patients according to the SM protocol. For each MWSH patient, the demographics, peri-, intra-, and post-operative clinical features were collected prospectively (63% of the cases from September 2016) or retrospectively, after which they were recorded in an institutional board-approved Microsoft Excel database. The following characteristics were included: sex, age, body mass index (BMI), Class of obesity according to the World Health Organization classification for obesity (Class I BMI 30.0-34.9 kg/m2, Class II 35.0-39.9 kg/m2, Class III 40.0-49.9 kg/m2, [26]). The following characteristics were also included: the American Society of Anesthesiologists (ASA) class. The author defined the hernias "MWSH" when they were widely spaced and/or often located at the opposite ends/sides of the abdominal-wall (see YouTube videos) and needed to be repaired in a single operation with multiple (2 or more) SMs. It was technically impossible to repair them with a single mesh, including cases of only 2 MWSH. He divided MWSH patients into Group 1, including the triple VH, and Group 2, including the double VH. Group 1 consists of two subgroups: subgroup 1 with wide spaces between the VH that need to be repaired with 1 SM per hernia; subgroup 2 with triple VH, when one is widely isolated from a cluster of two, all 3 VH require repair with 2 SM: 1 for the isolated hernia, and 1 for the cluster of two. S.A.C. put a patient into Group 2 when he had a double VH with wide spaces between them that needed to be repaired with 1 SM per hernia. The MWSH were "non-contralateral" when they were located in the same half-part (left or right) of the abdominal-wall (AW) and/or at its center; and "contralateral" when located in both half-parts of the AW (Figure 1, see YouTube videos); one or more widely-spaced VH may also be present at the center of the AW. Other variables were VH type (incisional or primary); preoperative size of fascial defect at physical examination (PE); VH neck-size according to AW ultrasound (US) and/or CT-scan; VH operative neck-size and type (small/medium [S/M] and large [L]) - according to Korenkov, et al.'s Classification and surgical treatment of incisional hernia [27]; the author considered a VH to be giant (G) or massive (M) when its diameter was 15-19.9 cm or ≥ 20 cm respectively, both without loss of domain, when the VH was oval, he measured the major axis [24]; massive (M) without loss of domain (≥ 20 cm); satellite VH; DR, which were considered a widening of the line a alba exceeding 2 cm [13]; mesh-type employed (composite or non-composite); type of fixation device employed; operation time; estimated blood loss at suction; operative complications; possible conversion to open surgery; early postoperative complications (within 30 days after operation); readmission to hospital; reoperation; postoperative day when patient returns to regular diet; length of hospital stay; chronic AW pain when it lasted > 3 months [28]; and the final outcome at follow-up (F.U.). The results were expressed as a mean ± SEM (SD) and as a percentage (%). The operation time for Groups 1 & 2 was compared. As a routine follow-up at our Institute, MSM patients were called for the out patients interview, which included a PE, at 1 and 4 weeks and 3 months postoperatively. The same interview, plus a review of AW US results, was scheduled for 6 months after the MSM operation, and then yearly.
SM surgical technique: Physical & chemical principles of SM surgical action
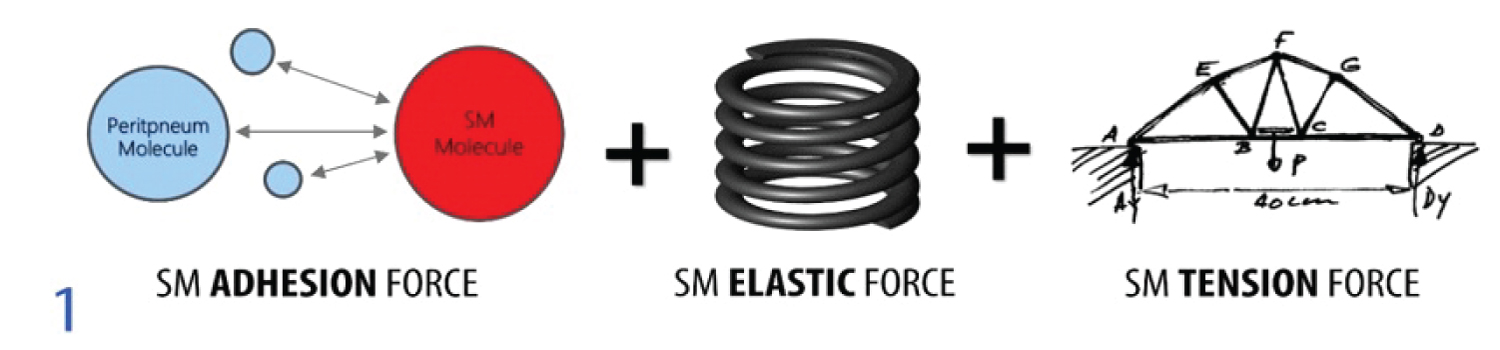
• A SM's adhesion force is a complex physical and chemical phenomenon of an electrostatic nature which is produced during the molecular attraction between two types of solid that come into contact, such as a SM and the parietal peritoneum. A similar example would be in cell biology of embryogenesis, when adhesion is the mechanism by which cells unite with each other, or with an extracellular matrix (Figure 1), [24].
• A SM's elastic force is the physical and chemical phenomenon due to the shape memory of a mesh prepared as a SM which spontaneously unrolls when the polypropylene 3-0 fixing stitches are cut. In fact, when a SM is rolled up tightly and fixed with stitches, it is tightly compressed; consequently, its shape memory stores an elastic force similar to a spring being compressed between our fingers. The elastic force is slowly released and the mesh remembers its rolled shape when the surgeon cuts the stitches and the SM gently unrolls. The same force is generated when we spread our fingers, releasing the spring (Figure 1) [18,24].
• A SM's tension force is the physical and chemical phenomenon that enables the SM to self-sustain when is unfolded, stretched and fixed to the two opposite edges of the AW defect. In a similar example, tension force is generated when a bridge is built over a river and its tie rods are stretched and fixed between the two opposite banks (Figure 2) [18,24].
During a single operation using MSM, these 3 forces act simultaneously for each SM, generating a combined triple action which produces the well-known spring/self-supporting effect for each SM. This effect helps surgeons during all the meshes' fixation maneuvers and removes any need for time-consuming manipulation in association with the SM's typical increase of the intra-abdominal visibility and operating space for each SM fixation [18,24].
SM Surgical Technique: Planning for MWSH correct pre- and intraoperative diagnosis and for pre-MSM-fixation to ensure ergonomic trocar placement and MWSH repair:
in order to:
A. Study preoperatively MWSH with CT-scan.
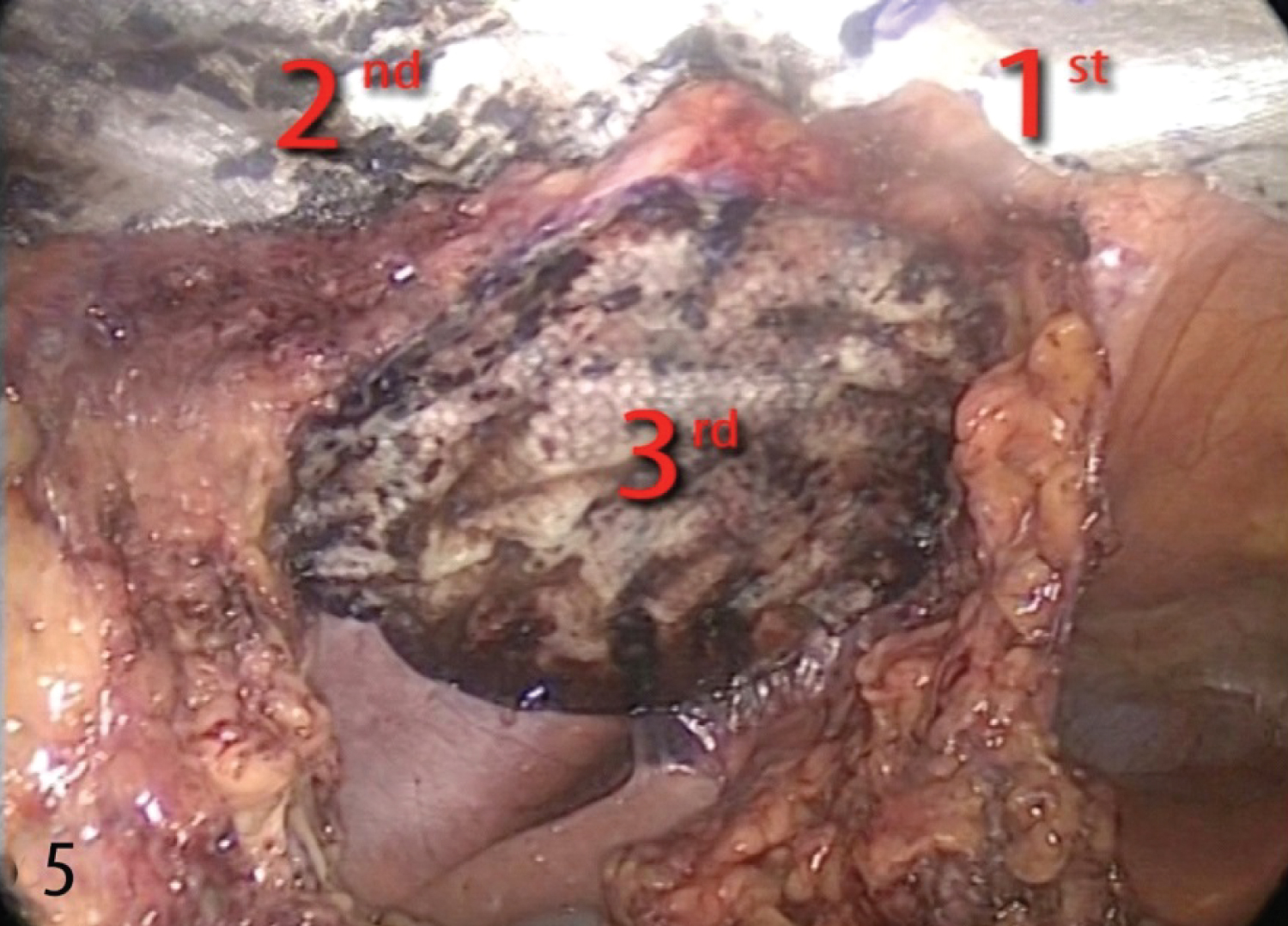
B. Identify all MWSH and any DR abdominis with adhesiolysis when necessary, and explore the entire AW during first laparoscopic step or phase 1 of the SM operation (Figure 3), see YouTube video. Plan ergonomic repair of all MWSH, keeping the area around each hernia free because a mesh must not block trocar placement.
C. Calculate optimal SM overlap for each VH and any DR pre-MSM-fixation.
D. Calculate ergonomic order of all trocar placements/removals to use as few as possible pre MSM-fixation, reducing the risk of tissue injury factors causing similar fascial wearing and future hernias (see YouTube video).
E. Calculate exact no. of trocars pre MSM-fixation.
F. Repair more than one non-contra lateral VH with the same trocars (No. 3-4) if possible.
G. Repair contra lateral VH with multiple trocars (No. 5).
H. Consider removing some trocars during operation to help the MWSH repair.
I. Repair MWSH and any DR with MSM, ensuring optimal SM overlap.
J. Repair any DR without using additional SM.
Results
There were 6 males and 2 females with MWSH with age and BMI averaging 57 ± 6 years (mean ± SEM; range 33-82 years) and 30 ± 2.7 kg/m2 (mean ± SEM; range 22-43 kg/m2). All patients underwent MSM repair. The cohort's demographics and pre- and operative features are detailed in Table 1. Thirty-eight percent of patients were obese. Sub group 1 of Group 1 comprised one case (Table 1) with triple VH who required repair with 3 SM. Subgroup 2 of Group 1 comprised 2 cases with triple VH: All 3 VH required repair with 2 SM: 1 for the isolated hernia, and 1 for the cluster of two (Table 1)]. The pre-operative and operative clinical features of Group 2 are detailed in Table 1 and Table 2. All 5 patients of Group 2 were operated on with 2 SM. Table 2 reports the MWSH pre-operative and operative clinical features of all 8 cases, including a comparison of the pre-operative and operative MWSH measurements. It also reports cases when laparoscopy detected additional spaced VH. During the operation, S.A.C. also found and repaired associated DR in 3 Group 2 cases, doing so without using additional SMs (Table 1 and Table 2). Operation time results are shown in Table 1. The mean ± SEM length of hospital stay was 3 ± 0.3 days, and 88% of patients resumed oral intake during the first postoperative day. In December 2021, the last follow-up was completed, with a minimum of 2 years after surgery. During a mean ± SEM follow-up of 72 ± 17.2 months (range, 24-145 months); all 8 MSM patients received a check-up with routine evaluations according to the aforementioned follow-up program. The author had no early - or late postoperative complications, chronic AW pain or VH recurrence.
Discussion
The multiple widely-spaced ventral hernias (MWSH) do not represent a single-organ disease as is usually found in various fields of surgical care. Being a poly district disease of the abdominal-wall (AW, see YouTube video), MWSH require much more attention in diagnosing and care than a single VH, especially if they are associated with diastases recti (DR). The difficulties surgeons face in treating MWSH increase as their number increases, especially when they do not know of their existence and/or underestimate their real number during the preoperative study (Figure 2) (see YouTube videos). In addition, in our experience, these difficulties increase further when MWSH are contra lateral in the AW because they require more ports for their repair than non-controlateral ones also considering the presence of the first "Slim-Meshes" (SM) already fixed to the AW during the operation. MWSH differs from the well-known "Swiss cheese ventral hernia" which generally can be repaired with a single mesh. We reinforce the idea that MWSH are widely spaced and/or often located at opposite ends/sides of the abdominal-wall (see YouTube videos) and it is impossible to repair them with a single mesh. It is impossible to define the distance between hernia defects that the surgeon should consider repair with a single mesh because the distance depends on case-to-case basis, the hernia neck-size and the mesh overlap. MWSH are found rarely (7%) in the treatment of ventral hernia (VH) patient, but they make surgery very insidious and not straightforward if the surgeon doesn't know of their existence. The MWSH group (8 patients) account for 7%, including some obese patients. It was a small, select group because the patients were chosen from the total number of SM cases and at our Department different types of surgical diseases are treated. During laparoscopy (LAP) S.A.C. found additional spaced VH [17-25] in 3 patients, who had a mean BMI of 31 kg/m2. This means, in his experience, a surgeon should be prepared to think intra-operatively about the repair of undetected MWSH (Figure 2, see YouTube video). There are no data in literature on the LAP treatment of MWSH and he had to devise and test a best diagnostic and therapeutic LAP approach, exploiting the benefits of LAP, plus the technical innovation and reliability of the SM technique. In the present study, the author analyzed the results from a decade of experience (between September 2009 and December 2019) with 8 MWSH patients treated with the novel SM technique using successive multiple SMs (MSM) during the same operation, thus confirming the SM's technical feasibility and innovation for the above particular and unknown patient-type. In his experience, he found CT-scan underestimated the real number of MWSH (Figure 2) and real VH neck-size in 3 and 1cases respectively; never the less, CT-scan is mandatory for MWSH preoperative study and should be supplemented with LAP findings to finalize the correct diagnosis and treatment for all the MWSH present in the same patient (Figure 2), [17-25]. In fact, we need to consider that a VH originates naturally from the inside of the abdomen and pushes outwards through the AW, which can hide it [22,24], especially in cases of obese patients (O) Class I-II. This has been shown to be even more so in cases of Class-III and super O ones, as their AW is thicker [22]. The author has already stated the difficulties surgeons face when they carry out physical examinations (PE) on VH O/super O and the role of LAP leading to the optimal VH internal viewing [22-25], which is more natural and accurate than the external ones, such as PE, AWUS and AW exploration conducted by the surgeon before open VH repair. Only after correct LAP identification of the MWSH's real number and their exact AW position can surgeons plan ergonomic trocar placement and pre-MSM-fixation maneuvers for MWSH repair. In fact, during operation they need to plan consecutive MSM repair using the fewest number of trocars and imagine their correct placement in the AW by numbering them precisely (see SM technique YouTube). Following planning of MWSH repair, surgeons can also consider removing some trocars in order to optimise MSM fixation make over's (see SM Technique YouTube video). Moreover, even in cases of MWSH LAP repair, the SM technique proved to be safe and straightforward. In fact, it eliminated the multiple sets of transabdominal full-thickness stitches used in traditional LAP VH repair, meaning zero related intra- and postoperative complications (up to 55% for one set), for example hematomas [29], organ iatrogenic injuries, intraoperative bleeding, chronic postoperative pain, mesh breakdown, suture site infections [30], cosmetic damage [17,18,22,24].
In addition, the reason why S.A.C. use the SM technique for MWSH repair is that MSM are slim and compact, thus increasing intrabdominal visibility and operating space which is raised to the AW front and well-clear of organs, reducing the risk of causing iatrogenic injuries when maneuvering MSM consecutively, both blind and on camera [17-25].
This increased visibility led to straightforward calculation of overlap size for all MSM during fixing maneuvers, ensuring optimal unrolling and tensioning without wrinkles, and reducing intra- (0%) and postoperative complications [17-25], for example chronic AW pain (0%) and VH recurrence (0%).
The SM technique reduced the risk (0%) of converting to laparotomy (up to 10% for each set of transabdominal full-thickness stitches) [31]. It also proved to be fast, even for MWSH patients with an overall mean operation time of 153 minutes. There are no data from the literature on MWSHLAP repair, so a comparison with this result is impossible.
Additional prospective studies are needed to draw further conclusions about the care of MWSH patients. In conclusion, this study reveals the existence of a new patient-type, namely one with MWSH. In the author's experience, the SM technique facilitates intra-abdominal introduction, orienting and fixation of successive MSM in the same MWSH patient, proving to be safe, straight forward, fast, economical and also affordable [22-25] (Figure 4 and Figure 5).
Acknowledgements
The author thanks Andrew Bailey for his supervision of the English version and Stefano Varotto for his collaboration in editing the photographs.
Author Contribution
S.A.C. invented the "Slim-Mesh" technique in 2009, was the responsible of the clinical management and wrote the manuscript.
Disclosure
The author reports no conflict of interest.
Funding
None to disclose for the author.
References
- Shian B, Larson ST (2018) Abdominal wall pain: Clinical evaluation, differential diagnosis, and treatment. Am Fam Physician 98: 429-436.
- vanRooijen MMJ, Lange JF (2018) Preventing incisional hernia: Closing the midline laparotomy. Tech Coloproctol 22: 623-625.
- Nevo N, Goldstein AL, Yakubovsky O, et al. (2021) How-we-do-it: The repair of postoperative ventral hernias after a Mercedes abdominal incision. Langenbecks Arch Surg 406: 2117-2123.
- Bravo-Salva A, González-Castillo AM, Vela-Polanco FF, et al. (2020) Correction to: Incidence of incisional hernia after emergency subcostal unilateral laparotomy: Does augmentation prophylaxis play a role? World J Surg 44: 3960-3962.
- Ho J, Richardson JK (2015) Rectus abdominis denervation after subcostal open laparotomy. Am J Phys Med Rehabil 94: e43-e44.
- Furneaux RW (1973) Bilateral subcostal laparotomy for the correction of a diaphragmatic hernia. Can Vet J 14: 19-20.
- Kurze C, Keel MJB, Kollar A, et al. (2019) The pararectus approach - a versatile option in pelvic musculoskeletal tumor surgery . J Orthop Surg Res 14: 232.
- Marrs C, Blackwell S, Hester A, et al. (2019) Pfannenstiel versus Vertical Skin Incision for Cesarean Delivery in Women with Class III Obesity: A Randomized Trial. Am J Perinatol 36: 97-104.
- Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: A qualitative systematic review. Hernia 15: 113-121.
- Bosanquet DC, Ansell J, Abdelrahman T, et al. (2015) Systematic Review and Meta-Regression of Factors Affecting Midline Incisional Hernia Rates: Analysis of 14,618 Patients. PLoS One 10: e0138745.
- Van Silfhout L, Leenders LAM, Heisterkamp J, et al. (2021) Ventral Hernia Group Tilburg. Recurrent incisional hernia repair: Surgical outcomes in correlation with body-mass index. Hernia 25: 77-83.
- Novitsky YW, Cobb WS, Kercher KW, et al. (2006) Laparoscopic ventral hernia repair in obese patients: A new standard of care. Arch Surg 141: 57-61.
- Hernández-Granados P, Henriksen NA, Berrevoet F, et al. (2021) European Hernia Society guidelines on management of rectus diastasis. Br J Surg 108: 1189-1191.
- Canton SA, Pasquali C (2022) "Slim-Mesh" Technique for Giant Ventral Hernia. JSLS 26: e2021.00079.
- Alexander AM, Scott DJ (2013) Laparoscopic ventral hernia repair. Surg Clin N Am 93: 1091-1110.
- James TJ, Wu J, Won P, et al. (2022) Hernia-to-neck ratio is associated with emergent ventral hernia repair. Surg Endosc 36: 9374-9378.
- Strigård K, Clay L, Stark B, et al. (2016) Giant ventral hernia-relationship between abdominal wall muscle strength and hernia area. BMC Surg 16: 50.
- Pless TK, Pless JE (1993) Giant ventral hernias and their repair. A 10 year follow up study. Scand J Plast Reconstr Surg Hand Surg 27: 311-315.
- Canton SA, Merigliano S, Pasquali C, et al. (2016) Prosthetic mesh “slim-cigarette like” for laparoscopic repair of ventral hernias: a new technique without transabdominal fixation sutures. Updates Surg 68: 199-203.
- Canton SA, Pasquali C (2017) Laparoscopic repair of ventral/incisional hernias with the “Slim-Mesh” technique without transabdominal fixation sutures: Preliminary report on short/midterm results. Updates Surg 69: 479-483.
- (2018) 26th International Congress of the European Association for Endoscopic Surgery (EAES), London, United Kingdom, 30 May-1 June 2018 Poster Presentations. Surg Endosc 483-614.
- (2019) 27th International Congress of the European Association for Endoscopic Surgery (EAES) Sevilla, Spain, 12-15 June 2019 Surg Endosc 33: 485-781.
- (2020) 28th International Congress of the European Association for Endoscopic Surgery (EAES) Virtual Congress 23-26 June 2020 Surg Endosc 34: 1-166.
- Canton SA, Piotto A, PasqualiC, et al. (2020) The impact of the “Slim-Mesh” Technique on operation time and short/midterm outcomes in 67 overweight, obese and superobese patients from a 10-year follow-up study. J Metab Bariatr Surg 9: 24-32.
- (2021) The Society of Laparoscopic & Robotic Surgeons. Virtual SLS MIS 2021 Conference Abstract Supplement JSLS 25: 15.
- (2022) Abstracts from the 29th International Congress of the European Association for Endoscopic Surgery (EAES), Barcelona, Spain, 24-27 November 2021. Surg Endosc 36: 325-674.
- Wang S, Majumdar SR, Padwal R, et al. (2015) BMI, annual blood pressure measurements, and mortality in patients with obesity and hypertension: A retrospective cohort study. Blood Press Monit 20: 32-38.
- Korenkov M, Paul A, Sauerland S, et al. (2001) Classification and surgical treatment of incisional hernia. Results of an experts' meeting. Langenbecks Arch Surg 386: 65-73.
- Tsirline VB, Klima DA, Belyansky I, et al. (2013) Chronic pain after ventral hernia repair. In: Jacob B, Ramshaw B, The SAGES Manual of Hernia Repair.
- Bittner R, Bingener-Casey J, Dietz U, et al. (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias International Endohernia Society (IEHS)-part-1. Surg Endosc 28: 2-29.
- Zhang Y, Zhou H, Chai Y, et al. (2014) Laparoscopic versus open incisional and ventral hernia repair: A systematic review and meta-analysis. World J Surg 38: 2233-2240.
Corresponding Author
Silvio Alen Canton, Department of Surgery, Oncology and Gastroenterology, (DiSCOG), University of Padua, Padua, 35122, Italy, Tel: (+39)-0498213264, Fax: 0498213151.
Copyright
© 2023 Canton SA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.